Introduction
Sepsis is currently defined as a life-threatening organ dysfunction secondary to a dysregulated physiologic response to infection. There are widely used, evidence-based guidelines for diagnosis and management of sepsis in human medicine,1but there is no single guideline or consensus statement on sepsis management in veterinary medicine. The guidelines most veterinarians follow, and those which we use at my hospital, are derived from expert opinion and the adaptation of human sepsis protocols employed at several academic veterinary institutions.
Management of sepsis is a great example of the challenge of practicing evidence-based medicine in an evidence-poor environment. Extrapolation from evidence in humans and reasoning from physiologic first principles are rational and necessary strategies, but of course they sometimes lead to practices which turn out to be ineffective or even counterproductive in veterinary patients. Such approaches should always be viewed as a starting point, a provisional strategy pending the development of better evidence in clinical studies of the target patient population.
Human medicine, though often blessed with much higher quality evidence that we can typically expect, still finds itself mired in controversies over questionable practices that become widespread despite limited or poor-quality evidence and which later turn out to have been ineffective. A condition such as sepsis, which is acutely life-threatening and for which no universal, highly-effective therapy is yet available, is fertile ground for such disputed approaches. These often spill over into veterinary medicine when we adopt new practices in human patient care, and it is important for us to keep an eye on the evolution of ideas and evidence regarding such practices. In the case of sepsis, for example, the use of Vitamin C, alone or in combination with steroids and other vitamins, is an example of a controversial practice that has been ported into our patient care protocols to some extent based on limited, and controversial, early evidence and which we may now want to rethink.
Diagnosis of Sepsis
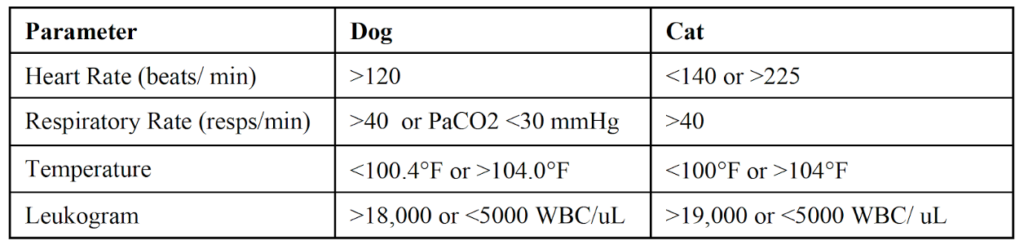
Confirming sepsis and identifying a source of infection can be challenging. However, the emphasis in sepsis management is now on early initiation of therapy since this has been associated with lower mortality in human patients, so diagnostic criteria have been developed to favor rapid diagnosis and therapy. Based on the definition of sepsis given above, a tentative diagnosis of sepsis should be made whenever there is a known or suspected infection and evidence of organ dysfunction or a systemic inflammatory response. Suspicion of infection should be based on history and physical examination findings. Suggested criteria for identifying organ dysfunction and an inflammatory response in dogs and cats, adapted from those used in humans, include:
Therapy
The emphasis on early intervention for sepsis has led to the development of treatment and monitoring “bundles,” that is sets of tests and treatments to be implemented universally when sepsis is suspected. There are no validated guidelines or consensus statements to define sepsis bundles in veterinary patients, however many institutions use treatment protocols adapted from those recommended for humans. The priorities for sepsis treatment are:
- Early institution of antibiotic therapy2
- Hemodynamic stabilization
- Identification and control of the source of infection
- Supportive care and recovery
Immediate Therapy for Sepsis
Following a tentative diagnosis of sepsis, recommended immediate care should include:
- Culture samples- Samples for culture should be obtained before antibiotic administration if this does not delay the use of antibiotics more than 45 minutes. Samples should be specific to the site of infection if this has been identified and can be accessed. If the site is unknown or inaccessible, blood cultures and urine cultures can be taken. Both aerobic and anaerobic cultures should be run.
- Antibiotics- A de-escalation approach is currently favored in the treatment of human sepsis patients. This involves early initiation of broad-spectrum antibiotic therapy and then a reduction in antibiotic coverage as soon as possible as indicated by culture results. Recommended duration of antibiotic therapy for humans is 7-10 days unless the source of infection cannot be definitively controlled
There are no evidence-based guidelines for antibiotic use in veterinary sepsis patients. Ideally, antibiotic selection should be based on culture results, local population susceptibility patterns, and the history and condition of the individual patient. Common empiric protocols used in veterinary sepsis patients include:
- Ampicillin/Unasyn + Amikacin
- Ampicillin/Unasyn + Enrofloxacin
- Cefazolin + Cefotaxime
- Cefoxitin
- Clindamycin + Enrofloxacin
- Lactate Measurement- Lactate is an important biomarker for sepsis management. Values > 2.5 mmol/L should be interpreted as an indicator of inadequate perfusion.
- Fluid therapy- Crystalloids are the initial fluid of choice, and aggressive fluid therapy (e.g. boluses of 20-30mL/kg over 15 minutes) should be initiated for patients with evidence of hypotension (e.g. MAP< 65mmHg) or poor perfusion (e.g. lactate > 4.0 mmol/L or consistent physical exam findings) unless there is a clear contraindication (e.g. primary cardiac disease, evidence of overhydration). Fluid therapy should be titrated to endpoints, including:
- Normalization of heart rate
- Normalization of respiratory rate
- Normalization of blood pressure (MAP> 65mmHg, systolic > 100mmHg)
- Normalization of lactate (< 2.0mmol/L)
- Normalization of mentation
- Normalization of urine output (UOP> 1mL/kg/hr)
Hetastarch is not recommended in human sepsis patients due to some evidence of increased mortality and risk for acute kidney injury. It is unclear the extent to which this applies to veterinary patients,3 however many experts recommend avoiding synthetic colloids if possible. Canine albumin is preferred as a colloid, though it is often unavailable or unaffordable.
Additional Therapy
- Continued hemodynamic stabilization- If the targets for fluid therapy (blood pressure, lactate, etc.) are not met with initial crystalloid treatment, vasopressors should be started early because hypotension in sepsis is often due to decreased peripheral vasomotor tone. Based on guidelines for humans and limited evidence in veterinary patients, the following are common recommendations for use of vasopressors in sepsis patients:
Warning! Some vasopressors can cause ischemic necrosis due to extreme vasoconstriction. They should ideally be given through a central line, and clients should be advised of this possible complication.
- Norepinephrine- 0.1-0.5mcg/kg/min Start low and titrate upwards in 0.1mcg/kg/min increments every 5-10 min until BP targets are reached (e.g. MAP>65mmHg) or 2-3mcg/kg/min is reached.
- Vasopressin is often recommended as a second-line pressor or to reduce the dose of norepinephrine in humans, but it is often unavailable to veterinary patients due to cost.
- Epinephrine- 0.05- 1mcg/kg/min. This can be added to norepinephrine if needed and titrated upwards every 5-10 min until BP targets are reached.
- Dopamine- This drug has historically been the pressor of choice in veterinary patients, but recent practice has shifted to norepinephrine based largely on extrapolation from research in human sepsis patients.
- Dobutamine- This is primarily an inotrope and is only recommended if there is evidence of poor contractility because it decreases vascular tone and can decrease BP
- Epinephrine- 0.05- 1mcg/kg/min. This can be added to norepinephrine if needed and titrated upwards every 5-10 min until BP targets are reached.
It is important to identify all physiologic abnormalities that can be treated in patients with sepsis and septic shock. These may include:
- Electrolytes
- Blood Glucose
- Lactate
- PCV/TP/albumin
- Coagulation- PT/PTT/platelet counts
- Blood Pressure
- Vital signs- HR, RR, body temperature, pulse quality, mm color, CRT
- SPO2
- ECG
- Pain Score and mental status- Analgesia should be provided if there is evidence of pain. NSAIDs should be avoided if there is hemodynamic instability or evidence of GI or renal impairments.
- Urine output and renal values
- Body weight- this is a key measure for assessing fluid balance
Other Therapies
- Gastroprotectants- (e.g. pantoprazole)
These can be considered if there is evidence of gastrointestinal lesions or symptoms - Anti-emetics- (e.g. maropitant, ondansetron)
These can be considered if there is evidence of nausea or vomiting.
- Promotility drugs- (e.g. metoclopramide, low-dose erythromycin) These can be considered if there is evidence of GI hypomotility or ileus.
- Blood products-
There is significant controversy and uncertainty regarding the use of blood products in septic patients. Strict arbitrary cutoff values for use of blood products are now discouraged in human patients due to growing evidence of harm related to transfusion. There are no clear guidelines for veterinary patients. - Treatment of Anemia-
Most critical patients become anemic at some point. Anemia should be treated when associated with significant clinical symptoms (e.g. hypoxia, tachypnea/tachycardia), ongoing losses of red blood cells, or anticipated losses associated with surgical source control procedures.. Though strict cutoffs are discouraged, a Hb of 7.0g/dL is often used as a guideline for when to transfuse in human sepsis patients. - Treatment of Thrombocytopenia-
Platelet-rich plasma is given to humans when there is clinical evidence of bleeding (e.g. petechiae, ecchymoses, epistaxis), when a surgical procedure is planned and platelet count is < 50k/mm3, or prophylactically when platelet count is <10k/mm3. - Treatmwnt of Coagulopathy- It is not recommended to give fresh-frozen plasma (FFP) to correct clotting times in the absence of active bleeding. If PT/PTT are elevated and there is bleeding or a surgical procedure is planned, FFP may be beneficial.
Vitamin C
Though this is, at best, an ancillary therapy to consider in patients with sepsis, without the acknowledged critical importance of many others and not necessarily widely used in veterinary patients, I want to focus a bit on it because it illustrates the challenges of an evidence-based approach to a complex medical problem.
In human medicine, as in the veterinary field, practices may be adopted based on early evidence that is both encouraging and extremely limited. Unlike veterinary medicine, however, follow-up studies are much more common and robust, and better evidence that shows the true state of affairs is often available within a few years. Unfortunately, in our profession we are more likely to adopt a practice based on a single small study and then employ it widely for a long time before subsequent studies either confirm the benefits or show them to be illusory. Vitamin C for sepsis is a cautionary tale that should encourage us to try harder to confirm our initial assessment of new therapies.
In 2017, a study of 94 human patients with sepsis was published comparing patient given standard treatment and those also given Vitamin C, thiamine, and low-dose hydrocortisone (called HAT therapy).4 This was a small by the standards of human medicine, though larger than many equally influential veterinary trials, but it appeared to show dramatic benefits. Mortality was 8.5% in the experimental group and 40.4% in the control group, and there were apparent benefits in terms of other standardized measures of disease severity.
This study had a dramatic impact in the human critical care field, with reverberations in veterinary medicine. Debate and additional research began immediately in human medicine. In the veterinary profession, there was buzz about this new treatment at conferences5 and online, and some veterinarians began adding it to their management of sepsis cases.6 It is unclear how widespread this practice became in veterinary circles, but the published research on Vitamin C in critically ill veterinary patients is pretty sparse, and there are not prospective randomized clinical trials specifically comparing HAT to standard care in veterinary sepsis cases.5–7
In contrast, the five years since the publication of the original HAT study has seen a flurry of research in humans, and there are now more than a dozen systematic reviews and meta-analyses evaluating studies in thousands of sepsis patients.4,8–17 Unfortunately, the majority of these have failed to confirm the dramatic results from the original study. Most have found no reduction in mortality from adding HAT to standard care. Some have shown modest improvement in some assessments of disease severity, but many have found no statistically significant nor clinically meaningful effect at all.
This is about as clear an example of the Decline Effect as one could ask for. Dramatic effects seen in initial studies of a new therapy get smaller and smaller as subsequent studies attempt to replicate the results until the literature settles on a far less dramatic reality, which surprisingly often turns out to be no effect at all. The explanations for this involve both intentional and, most of the time, unconscious bias on the part of enthusiastic researchers studying a new idea, as well as the limitations of small, often poorly controlled research studies in unrepresentative patient populations. This phenomenon is the main reason we should avoid enthusiastically embracing new therapies before appropriate replication of such initial studies has been done.
In the case of HAT, the controversy has grown more dramatic than usual. The primary author of the original study, Dr. Paul Marik, vehemently stands by his results despite all the failed attempts to replicate them. A recent letter to the editorof the journal in which this study was published has alleged that analysis of the results and statistics reported in the original paper is not only suggestive of data fabrication but clear proof of misconduct. An investigation by the journal is likely, especially in light of a very similar controversy involving the same investigator.
Dr. Marik has also published a study purportedly showing a different novel approach with equally dramatic benefits in COVID-19 patients. This paper has recently been retracted due to evidence of data manipulation. The author has also been reprimanded by the Virginia Medical Board for misconduct, resigned his academic position, and become involved in a lawsuit with his hospital over the use of ivermectin as a COVID-19 therapy. Like HAT, the approach Dr. Marik advocates for COVID-19 appeared promising in his early studies, but the elements of it have so far failed to show benefits in subsequent research.18,19 Dr. Marik illustrates starkly how hard the habit of excessive enthusiasm for new therapies based on preliminary evidence is to break.
Bottom Line
Sepsis is a serious and complex problem with numerous possible treatment approaches and mixed, often disappointing results. An evidence-based approach involves attention to the limited and weak evidence available in veterinary patients and judicious extrapolation from the more robust, but still imperfect, evidence available in humans.
The use of Vitamin C, alone or in combination, in sepsis patients has evolved from an exciting and promising new idea to an example of failed promise, and of the dangers of unconscious bias, if not outright scientific fraud. The lesson we should draw from this is not merely that use of Vitamin C in veterinary sepsis patients is probably not warranted, but that we should proportion our acceptance of and confidence in new therapies to the strength of the evidence for them. For veterinarians, this often means a perpetual state of using treatments in which we can have very little confidence, but this is still preferable to enthusiastic commitment to practices which later prove ineffective or even dangerous for our patients.
References
1. Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit Care Med. 2021;49(11):e1063-e1143. doi:10.1097/CCM.0000000000005337
2. Abelson AL, Buckley GJ, Rozanski EA. Positive impact of an emergency department protocol on time to antimicrobial administration in dogs with septic peritonitis. J Vet Emerg Crit Care. 2013;23(5):n/a-n/a. doi:10.1111/vec.12092
3. Glover PA, Rudloff E, Kirby R. Hydroxyethyl starch: a review of pharmacokinetics, pharmacodynamics, current products, and potential clinical risks, benefits, and use. J Vet Emerg Crit Care (San Antonio). 2014;24(6):642-661. doi:10.1111/vec.12208
4. Marik PE, Khangoora V, Rivera R, Hooper MH, Catravas J. Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study. Chest. 2017;151(6):1229-1238. doi:10.1016/j.chest.2016.11.036
5. Silverstein D. Treating Sepsis with Vitamins? The Risks, Benefits, and Evidence. In: International Veterinary Emergency and Critical Care Symposium. Washington, D.C.; 2019.
6. Taylor SD. Oranges for Horses? Exploring Vitamin C in the Fight against Equine Sepsis. Purdue Equine Heal Updat. 2019;21(2):5.
7. Gordon DS, Rudinsky AJ, Guillaumin J, Parker VJ, Creighton KJ. Vitamin C in Health and Disease: A Companion Animal Focus. Top Companion Anim Med. 2020;39:100432. doi:10.1016/j.tcam.2020.100432
8. Fujii T, Luethi N, Young PJ, et al. Effect of Vitamin C, Hydrocortisone, and Thiamine vs Hydrocortisone Alone on Time Alive and Free of Vasopressor Support Among Patients With Septic Shock. JAMA. 2020;323(5):423. doi:10.1001/jama.2019.22176
9. Anderson MJ, Ibrahim AS, Cooper BR, Woolcock AD, Moore GE, Taylor SD. Effects of administration of ascorbic acid and low-dose hydrocortisone after infusion of sublethal doses of lipopolysaccharide to horses. J Vet Intern Med. 2020;34(6):2710-2718. doi:10.1111/jvim.15896
10. Lee YR, Vo K, Varughese JT. Benefits of combination therapy of hydrocortisone, ascorbic acid and thiamine in sepsis and septic shock: A systematic review. Nutr Health. 2022;28(1):77-93. doi:10.1177/02601060211018371
11. Wu T, Hu C, Huang W, Xu Q, Hu B, Li J. Effect of Combined Hydrocortisone, Ascorbic Acid and Thiamine for Patients with Sepsis and Septic Shock: A Systematic Review and Meta-Analysis. Shock. 2021;56(6):880-889. doi:10.1097/SHK.0000000000001781
12. Assouline B, Faivre A, Verissimo T, et al. Thiamine, Ascorbic Acid, and Hydrocortisone As a Metabolic Resuscitation Cocktail in Sepsis: A Meta-Analysis of Randomized Controlled Trials With Trial Sequential Analysis. Crit Care Med. 2021;49(12):2112-2120. doi:10.1097/CCM.0000000000005262
13. Patel JJ, Ortiz-Reyes A, Dhaliwal R, et al. IV Vitamin C in Critically Ill Patients: A Systematic Review and Meta-Analysis. Crit Care Med. 2022;50(3):e304-e312. doi:10.1097/CCM.0000000000005320
14. Fujii T, Salanti G, Belletti A, et al. Effect of adjunctive vitamin C, glucocorticoids, and vitamin B1 on longer-term mortality in adults with sepsis or septic shock: a systematic review and a component network meta-analysis. Intensive Care Med. 2022;48(1):16. doi:10.1007/S00134-021-06558-0
15. Ge Z, Huang J, Liu Y, et al. Thiamine combined with vitamin C in sepsis or septic shock: a systematic review and meta-analysis. Eur J Emerg Med. 2021;28(3):189-195. doi:10.1097/MEJ.0000000000000812
16. Scholz SS, Borgstedt R, Ebeling N, Menzel LC, Jansen G, Rehberg S. Mortality in septic patients treated with vitamin C: a systematic meta-analysis. Crit Care. 2021;25(1):17. doi:10.1186/s13054-020-03438-9
17. Somagutta MKR, Pormento MKL, Khan MA, et al. The Efficacy of vitamin C, thiamine, and corticosteroid therapy in adult sepsis patients: a systematic review and meta-analysis. Acute Crit care. 2021;36(3):185-200. doi:10.4266/acc.2021.00108
18. Popp M, Stegemann M, Metzendorf M-I, et al. Ivermectin for preventing and treating COVID?19. Cochrane Database Syst Rev. 2021;(7). doi:10.1002/14651858.CD015017.PUB2
19. Lim SCL, Hor CP, Tay KH, et al. Efficacy of Ivermectin Treatment on Disease Progression Among Adults With Mild to Moderate COVID-19 and Comorbidities. JAMA Intern Med. 2022;182(4):426. doi:10.1001/jamainternmed.2022.0189


Did you miss out the criteria for identifying sepsis in cats and dogs? Or am I missing where they are?
yes, looks like the image didn’t upload. Thanks for catching that!
Pingback: ? Un enfoque racional y la controversia de la vitamina C |