I recently gave a lecture at a continuing education conference looking at how the regulation of veterinary treatments works, and how vets can use this process to help them make evidence-based treatment recommendations. Understanding what is required to claim a treatment is “FDA approved,” and what it means when a product is not, is also useful for pet owners considering their options.
Making Evidence-based Treatment Choices
The core of evidence-based medicine is integrating the best current scientific evidence with our own clinical expertise and the needs of the patient and the client when making diagnostic and treatment recommendations.1 Accurately understanding the potential risks and benefits of a treatment is necessary for us to guide clients in making choices about their pets’ care.
However, it is impossible for each of us to be an expert on all the treatments available to choose from, and the time needed to keep current with the complex and expansive body of research evidence can be prohibitive. Clinicians frequently use shortcuts or proxies to help us understand how much confidence we can have in a given therapy and how much scientific uncertainty there is about it.
One of these proxies is the degree of regulatory evaluation and oversight applied to a product. There are different general categories of medicines available for vets and pet owners to choose from, and understanding the differences between these categories, including the evidence available supporting the safety and efficacy of each, can be a useful aid in evaluating our treatment choices.
A relatively new category of regulatory approval is Expanded Conditional Approval (XCA).2 In the last few years, some useful new drugs have become available to veterinarians through this pathway, such as Laverdia and Panoquel. Some not-so-new drugs have also been approved under this process, such as Vetmedin and potassium bromide. But what is conditional approval? How is it different from “regular” FDA approval?
This session will review the broad general categories of treatments available (in terms of regulatory oversight), with special focus on XCA and how vets can explain the significance of these categories to clients.
What Are Our Options?
In general, vets can choose among medicines in several broad categories:
- Prescription drugs fully approved under the supervision of the Food and Drug Administration’s Center for Veterinary Medicine (the FDA CVM)*
- Prescription drugs conditionally approved under a formal FDA process
- Drugs approved for use in humans or other species and used “off label”† in dogs
- Dietary supplements or other non-prescription treatments not tested or approved under a specific regulatory process
*Some veterinary products are regulated by other agencies, such as certain parasite preventatives (EPA) and vaccines (USDA), but FDA is responsible for approving most prescription drugs.
†”off label” is a common term vets use to describe what the FDA more often calls “extra-label” drug use. I explain the details of what this means a bit later.
There is also a category of fully approved drugs that can be labeled for use without the supervision of a veterinarian.13These over-the-counter (OTC) drugs have the same approval requirements as prescription products, but the manufacturer has demonstrated to the FDA that the drug can be safely and effectively used without supervision by a veterinarian, relying only on the directions on the label, so a prescription from a vet is not required. (This is slightly different from the process for approving OTC drugs for human use, which does not always require a regular drug approval process.)14
In general, the strength of the evidence identifying both the benefits and the risks of these treatments in the target species is greater the closer to the top of the list they are. For example, it takes a lot more research and data in dogs to achieve FDA approval for a prescription medication to be used in dogs than is required for a human drug used off-label or for a dietary supplement.
The FDA has legal authority to set the conditions for the use of any “drug,” which the agency defines as anything “intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease” and anything “(other than food) intended to affect the structure or any function of the body.”3 The agency regulates drugs for both humans and other animals, but the guidelines are often different depending on the species a product will be used in.
The categories of available treatments reflect the need for a compromise between the best possible evidence and the availability of treatments. Ideally, every medicine would go through the rigorous testing required for a fully approved prescription drug, or even more than that! However, this is a lengthy and expensive process, and a strict requirement to have this level of evidence for everything would drastically limit the treatment options available for vets and dog owners. Therefore, the FDA allows vets to use products other than approved prescription drugs. The agency also sets specific guidelines for each category to minimize the potential risk associated with the greater uncertainty in categories that require less extensive pre-approval testing.
This is helpful to veterinarians because it gives us more treatment options, but it also requires us to understand, and explain clearly to clients, the differences between these categories and what this means for how confident we can be in the safety and effectiveness of different types of treatments.
Fully Approved Prescription Drugs
The highest bar for scientific evidence is set by full FDA drug approval. This is a complex process that requires demonstrating to the agency that a drug proposed for use in dogs is safe, for the dogs taking it as well as for the humans around them, and that it is effective, meaning it consistently does what it is expected to do. Full approval requires showing that a drug can be consistently made to a high standard of quality. The FDA also has specific requirements for labeling the drug, for disclosing the evidence produced to support approval, and for what a company can and cannot claim about the drug once it is approved.
The major components of FDA approval for animal drugs are called the major technical sections. These include:3
- Target Animal Safety (TAS)
- Effectiveness
- Human Food Safety
- Chemistry, Manufacturing, and Controls
- Environmental Impact
Of greatest interest to clinicians are the TAS and effectiveness sections because these relate directly to our assessment of the potential risks and benefits of a drug for our patients. The TAS typically involves testing the drug at both the intended label dose and higher doses in healthy animals of the species for which the drug is intended. This helps establish the potential side effects of a drug and gives a sense of the “safety margin” or possible consequences of exposure to doses higher than the label dose or of using the drug in animals that are not healthy or may be especially sensitive in some way.
Effectiveness is often determined in a field study, which is usually a randomized, blinded, controlled clinical trial of the drug in individuals of the target species with the condition the drug is meant to treat. Such trials are conducted with oversight by the FDA, including review of the methodology before the study is run and review of the data after it is completed. This oversight helps reduce the influence of bias on the results.
All research studies involve bias, processes which systematically influence the design, conduct, or analysis of a trial in ways that alter the outcome. It is well-known, for example, that studies funded by industry are more likely to produce results favorable to the study sponsors than independently funded research.4 This is sometimes misunderstood as meaning that companies or researchers deliberately “fudge” the data to get the results they want, but that is rarely how bias works.
Most of the time, bias in research takes the form of small, unconscious effects on the numerous decisions that must be made at every step of designing and conducting a study and analyzing the data. Such processes are just as problematic when they involve ideology (e.g. homeopaths rarely conduct studies that show homeopathy doesn’t work), career advancement, or factors other than financial interests.5
Such biases occur in every study, and the classic research methods of randomization, blinding, and placebo controls are a few of many scientific methods that help minimize the influence bias has on the outcomes of research studies. Independent regulatory oversight, as is part of the FDA drug approval process, is another useful tool in minimizing the influence of bias on study results, and it allows us to have greater confidence in the findings of such clinical trials.
The FDA also requires companies marketing prescription drugs to monitor the experience that patients and vets have using the drug and submit regular reports after the drug comes on the market. This further strengthens our ability to identify and fix any problems once a product is in regular clinical use.
Of course, no scientific or regulatory process is ever perfect. Biology is complicated, so the effects of drugs are also complicated and never completely predictable. However, the standard of FDA approval is rigorous, and an approved prescription drug has been tested extensively and has more scientific evidence to support safety and efficacy than other categories of treatments available to us.
Expanded Conditional Approval- XCA
Established in 2018, the expanded conditional approval process is a relatively new regulatory category which recognizes that for conditions that are serious or life-threatening and for which there is no existing effective treatments, a quicker process that makes new drugs available for vets to use sooner is beneficial.1,6 The clinical studies needed to demonstrate effectiveness under the full approval process can be lengthy and complex for some kinds of drugs, and while these studies are necessary, patients may go for years without treatment while waiting for such research to be completed.
XCA is available for drugs intended for use in the seven designated “major species” (horses, dogs, cats, cattle, pigs, turkeys, and chickens) if they meet two core criteria:
- They are intended to address a serious or life-threatening condition, but demonstrating effectiveness would require complex or particularly difficult studies
OR - They address an unmet animal or human health need, but demonstrating effectiveness would require complex or particularly difficult studies
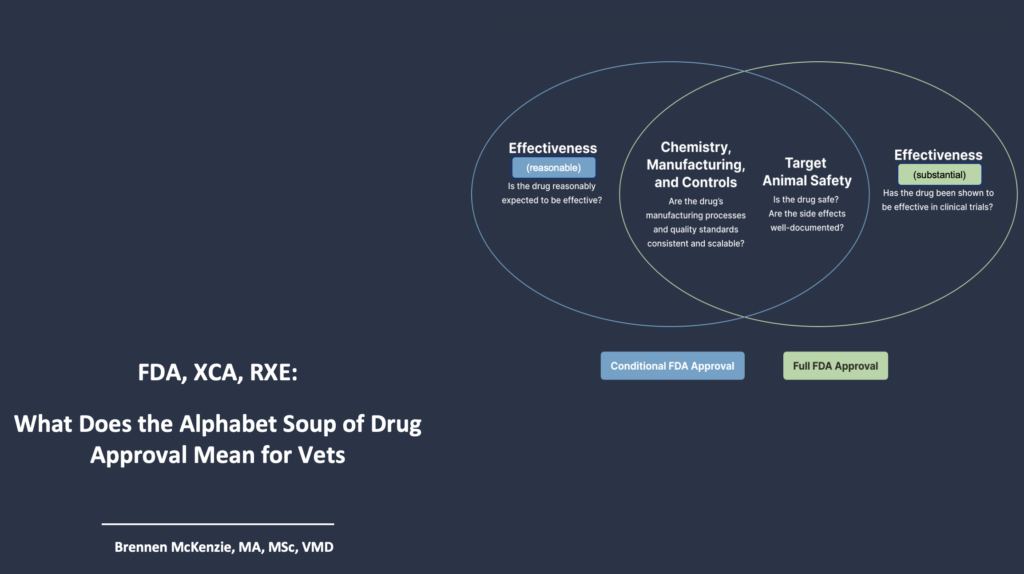
XCA requires most of the same evidence needed for full approval, including all of the major technical sections except for the usual effectiveness package. Therefore, confidence regarding safety and manufacturing quality can be just as high as for fully approved products. Evidence is still needed to establish effectiveness, but the specific standard is different.
Under XCA, rather than the “substantial evidence” for effectiveness standard, which typically requires a clinical trial in the target species, expanded conditional approval requires a “reasonable expectation of effectiveness” (RXE). This standard can potentially be met with studies that involve fewer dogs and shorter time periods than the clinical trials needed for full approval or with evidence already existing in the scientific literature from studies done previously. This shortens the time necessary to achieve approval which should ideally make it possible to bring needed products into use faster.
The XCA process is not intended to permanently replace the standard approval requirements. Unlike full approval, conditional approval is limited to one year. It is possible to renew XCA annually for up to five years so long as the company marketing the drug is making progress in generating the evidence required to meet the substantial evidence standard. Ultimately, the drug must be given full approval once this evidence is provided and accepted by the agency, or it must be withdrawn from the market.
A number of novel drugs have been approved under the XCA process, such as Laverdia (verdinexor) for treatment of lymphoma in dogs7 and Panoquel (fuzapladib) for management of canine pancreatitis symptoms.8 However, some drugs that have already been in widespread use under a different category, such as off-label use of products approved for humans or other species, have also been given XCA for specific uses in dogs.
Vetmedin (pimobendan) was fully approved for treatment of congestive heart failure (CHF) due to mitral valve disease (MMVD) or dilated cardiomyopathy in dogs in 2007 (and the generic version was approved for this indication in 2024).9,10 However, Vetmedin was approved conditionally under XCA in 2022 for use in ACVIM Stage B2 MMVD cases to delay the onset of congestive heart failure.11 The drug is the same, but the indication is different, and it is approved for CHF and pre-clinical MMVD under two different regulatory processes.
There are some differences in the rules for use of drugs that are fully approved versus those approved under XCA. The most significant is that vets cannot use a conditionally approved drug off-label, meaning for any purpose or in any way other than what is dictated by the label directions. For example, if a drug is only conditionally approved to treat staphylococcal skin infections in adult dogs, it would not be legal to use the drug to treat a urinary tract infection, a puppy, or a cat.
This restriction applies even if there is reason to believe the drug might be effective for these other uses, such as published research literature or anecdotal reports of such uses. This is a major difference from fully approved drugs, which sometimes can be used off label. Fortunately, it is easy for vets to recognize a conditionally approved drug because these will have the designation “CA” as part of the name (CA1 for the first conditionally approved use, CA2 for the second, and so on).
The XCA process allows needed treatments to be available to patients more quickly but also ensures a high standard of evidence. Vets using conditionally approved drugs can be confident that the evidence for safety is as robust as for any other drug, and the evidence for effectiveness is strong, though not as extensive as for a fully approved drug. Understanding this, vets can counsel their clients about the differences between full and conditional approval so owners can make informed choices about the risks and benefits of these treatments.
Off-label Use of Drugs Approved in Humans or Other Species
Many more drugs are approved and available for use in humans than in dogs, obviously because the biomedical industry for humans is much larger and better funded than veterinary medicine. The FDA recognizes that many potentially beneficial drugs are available in people, or other species, that will never be put through the approval process for use in dogs due to limitations of time, money, or other factors. Since 1994, the agency has allowed vets to use these drugs under specific conditions, and this is known as “extra-label” use (more commonly called “off-label”).12
Because the testing required for approval of a drug used off label was not specifically meant for the species or indication a clinician intends to treat, the approval data are less reliable indicators of how safe and effective the drug will be for this new use. As we all know, extrapolation across species is a necessary evil in veterinary medicine, but there are plenty of cases in which a drug that is safe and effective in one context may be neither in another. Tylenol is safe enough to be designated an over-the-counter (OTC) medication in humans, but it must be used with great caution in dogs and never in cats!
In recognition that the standard of evidence supporting off-label use of approved drugs is lower than for drugs fully or conditionally approved for the target species and indication, the FDA has set some rules for extra-label drug use.
Veterinarians must, of course, have an established veterinarian-client-patient relationship (VCPR) in order to prescribe a drug off-label, just as they should for any medical treatment. The FDA provides a set of criteria for the existence of a valid VCPR:
- you have recently seen and are personally acquainted with the keeping and care of the animal by virtue of examination or, for food animals, a visit to the place where the animals are housed
- you have assumed responsibility for making medical judgments about the health of an animal, and the owner has agreed to follow your instructions
- you have sufficient knowledge of the animal to form at least a general or preliminary diagnosis of the medical condition
- you are readily available for follow-up in case of adverse reactions or treatment failure.
In addition to establishing a valid VCPR, vets can only use an approved drug off label when an animal’s health is threatened or where the animal may suffer or die without treatment.
Off-label use of such treatments for cosmetic or performance enhancement purposes would not be allowed. Because the confidence we have in the safety and effectiveness of drugs used off-label is lower, the risks are considered greater, and thus there must be a meaningful need to justify taking those risks.
Vets also cannot use a drug off-label when there is an equivalent drug already approved for dogs, unless they determine that the approved drug is not appropriate or effective for a specific patient. Exactly what is necessary to determine this is not spelled out, so there is some uncertainty and room for discretion here. There are also detailed requirements for record-keeping, labeling, and compounding of drugs used off label.
Extra-label use of drugs approved for humans is one of the most common types of medication use in veterinary medicine. We understand that the evidence for safety and effectiveness in our patients is not as strong as it is for approved animal drugs, but these drugs are an indispensable clinical tool. As long as we, and our clients, understand the limits of the evidence, we can balance the potential risks and benefits, and the limits of the evidence, in a rational way and monitor patients appropriately.
Supplements
Dietary supplements are the category with the least oversight and the greatest uncertainty about safety and efficacy. In veterinary medicine, this is not even an official category. As the FDA explains, “there is no ‘dietary supplement’ regulatory classification for animal food substances and products.”15 The law that regulates dietary supplements for humans, the Dietary Supplement Health and Education Act of 1994 (DSHEA) has been ruled not to apply to veterinary species. Products marketed for these species “are considered either ‘foods’ or ‘new animal drugs’ depending on the intended use.”15
Essentially, anything that is intended to cure, treat, or prevent disease is considered a drug and should, in principle, go through the process for full or conditional approval before being marketed for use in companion animals. Some health claims are allowed for therapeutic diets, if they can be supported with evidence, but these are limited. Despite complex legal language and some degree of uncertainty, the bottom line is that food is food and medicine is medicine. If something is meant to be used as medicine, then it is a drug and not food. Foods don’t need to be approved by the agency before being marketed, but drugs do.
In practice, the FDA does not aggressively enforce this policy, and it typically does not insist on removal of supplements marketed for pets even if they have not been through the required drug approval process. In the past, the agency had an articulated policy indicating it would not object to marketing of pet supplements so long as they did not claim to treat or prevent disease or make other inaccurate claims and so long as there was no specific evidence suggesting they were harmful.16 That policy was withdrawn in early 2020, so exactly how the agency views regulating these products at this point isn’t entirely clear.17
The importance of this for veterinarians is that we must be aware that supplements for pets aren’t required to prove they are safe and effective before, or after, being marketed. Most of these products have never been tested in clinical trials, and the few studies that are done are typically set up and run by the company selling the product without any independent supervision. These studies can be interesting, but not surprisingly they often come up with results favorable to the company, and without the independent FDA monitoring, it is harder to be confident that these results are objective and unbiased.
There is also no official regulatory monitoring of quality for most dietary supplements. One study found, for example, that the labels for many probiotic supplements were inaccurate—often the products didn’t have the species or amount of probiotic organism claimed on the label.18 Similar results have been found for tests of other supplements.16
Even if a specific supplement might have therapeutic effects, your patients won’t benefit from these if the product you use doesn’t actually contain the ingredients it’s supposed to have! There are voluntary industry groups that make some effort to establish guidelines for supplement quality, but these are not mandatory nor independent of the manufacturers.
There may be research evidence relevant to determining the safety and efficacy of specific dietary supplements intended for companion animal species. However, the research is often sparse and rife with potential bias and error, and independently evaluating it for every product is impractical for most veterinarians. The absence of a robust regulatory process for pre-market approval of such products leaves the veterinarian with less guidance and less confidence in these treatments than we can have in those that are subject to more regulatory oversight.
Bottom Line
Science is imperfect, and medicine is an imperfect science. No medical treatment, whether a prescription drug or a dietary supplement, is ever completely effective or completely safe for every patient. There is always some level of risk in doing anything in medicine, and this has to be balanced against the potential benefits of the treatment in the context of the degree of evidentiary uncertainty.
As veterinarians, we can only decide what is best for our patients on the basis of the best evidence we have, integrated with our clinical expertise and the needs and goals of our clients. Uncertainty is inevitable, but the more evidence we have, the less uncertainty there is and the easier it is to make confident recommendations. Understanding the different levels of regulatory oversight for various categories of treatments can help us assess the strength of the scientific evidence and the degree of confidence we can have in the medicines we recommend.
References
- Cockroft, P. Holmes, M. (2003). Handbook of Evidence-Based Veterinary Medicine. Oxford: Blackwell.
- U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM). Eligibility Criteria for Expanded Conditional Approval of New Animal Drugs Guidance for Industry. 2021. Accessed on July 18, 2024. Available at: https://www.fda.gov/media/130706/download
- U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM). From an Idea to the Marketplace: The Journey of an Animal Drug through the Approval Process. Accessed on July 18,. 2024. Available at: https://www.fda.gov/animal-veterinary/animal-health-literacy/idea-marketplace-journey-animal-drug-through-approval-process#approved
- Resnik DB, Elliott KC. Taking financial relationships into account when assessing research. Account Res. 2013; 20(3): 184-205.
- Simmons JP, Nelson LD, Simonsohn U. False-positive psychology: undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol Sci. 2011; 22(11): 1359-1366.
- U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM). Conditional Approval Process Explained. Accessed on July 18, 2024. Available at: https://www.fda.gov/animal-veterinary/resources-you/conditional-approval-explained-resource-veterinarians
- Anivive Lifesciences, Inc. Corrected Freedom of Information Summary Conditional Approval Application: Application Number 141-526. 2021. Accessed on July 18, 2024. Available at: https://animaldrugsatfda.fda.gov/adafda/app/search/public/document/downloadFoi/10270.
- Ishihara Sangyo Kaisha, Ltd. Freedom of Information Summary Conditional Approval Application Application Number 141-567. 2022. Accessed July 18, 2024. Available at: https://animaldrugsatfda.fda.gov/adafda/app/search/public/document/downloadFoi/13134
- U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM). Oral Dosage Form New Animal Drugs; Pimobendan. Fed Reg. 2007; 72(95):27733.
- Cronus Pharma Specialities India Private Ltd. Freedom of Information Summary ANADA 200-728. 2024. Accessed July 18, 2024. Available at: https://animaldrugsatfda.fda.gov/adafda/app/search/public/document/downloadFoi/15345
- Boehringer Ingelheim Animal Health USA, Inc. Freedom of Information Summary Conditional Approval Application Application Number 141-556. Accessed July 18, 2024. Available at: https://animaldrugsatfda.fda.gov/adafda/app/search/public/document/downloadFoi/12512
- U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM). The Ins and Outs of Extra-Label Drug Use in Animals: A Resource for Veterinarians. Accessed July 18, 2024. Available at: https://www.fda.gov/animal-veterinary/resources-you/ins-and-outs-extra-label-drug-use-animals-resource-veterinarians
- U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM). Frequently Asked Questions about Animal Drugs: What are the differences between an over-the-counter animal drug, a prescription animal drug, and a veterinary feed directive animal drug? Accessed July 18, 2024. Available at: https://www.fda.gov/animal-veterinary/safety-health/frequently-asked-questions-about-animal-drugs#difference
- U.S. Department of Health and Human Services Food and Drug Administration. OTC Drug Review Process: OTC Monographs. Accessed July 18, 2024. Available at: https://www.fda.gov/drugs/otc-drug-review-process-otc-drug-monographs
- U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM). Product Regulation. Accessed July 18, 2024. Available at: https://www.fda.gov/animal-veterinary/animal-food-feeds/product-regulation#:~:text=Thus%2C%20there%20is%20no%20%22dietary,intended%20use%20(see%20below).
- Finno CJ. Veterinary Pet Supplements and Nutraceuticals. Nutr Today. 2020;55(2):97-101.
- U.S. Department of Health and Human Services Food and Drug Administration Center for Veterinary Medicine (CVM). CPG Sec. 690.100 Nutritional Supplements for Companion Animals. Accessed July 18, 2024. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/cpg-sec-690100-nutritional-supplements-companion-animals-withdrawn-2202020
- Weese JS. Evaluation of deficiencies in labeling of commercial probiotics. Can Vet J. 2003 Dec;44(12):982-3.


Pingback: Librela (bedinvetmab) for Arthritis in Dogs: Is it Safe? |