What’s the Fuss About?
In May of 2023, the FDA approved a new treatment for osteoarthritis (OA) pain in dogs. This was Librela (bedinvetmab). A monoclonal antibody that targets nerve growth factor (NGF), Librela was a completely new category of treatment for OA pain in dogs. This was greeted with significant excitement because, although there are many treatments used for this condition (e.g. 1, 2), all of them have their pros and cons, and it is not always possible to adequately maintain comfort and function in every dog with existing tools.
That excitement has subsequently been diminished by emerging concerns about the safety of Librela. Reports of adverse effects to the FDA by owners and veterinarians, negative media coverage, formation of anti-Librela groupsonline, and even a lawsuit against the manufacturer have all left dog owners confused and frightened about the effects of this drug. So what is actually happening, and what should vets and dog owners do?
To begin with, we should consider the context. Osteoarthritis is a common and serious condition that causes significant pain and disability in aging dogs and can be a reason for euthanasia due to diminished quality of life. As mentioned, there are many therapies available for OA. Some are well-understood and there is strong scientific evidence to support their use, such as non-steroidal anti-inflammatory drugs (NSAIDs. See 3, 4, 5). The value of others is less clear (e.g. glucosamine, gabapentin, acupuncture). Other factors, such as obesity and activity level, also play a role in the management of OA.
No one treatment alone is going to be a perfect solution for all patients, and the best approach will vary with circumstances., The most effective and best studied pain relievers are NSAIDs. While these drugs do have potential risks, they are well understood and the vast majority of dogs with OA can benefit from them safely. However, there seems to be great anxiety among pet owners and even vets about NSAIDS, and an unfortunate reluctance to use them appropriately. This can lead to inadequate treatment of pain in individual dogs, or to the use of dubious or ineffective treatments. This reluctance is also part of why Librela was greeted with such enthusiasm when it was introduced. There was a hope, encouraged by the manufacturer, that this would be a safer alternative first-line treatment than NSAIDs.
Where We Started
So was such hope justified by the scientific evidence when Librela was first introduced? Well, sort of.
The initial data used to gain FDA approval did show evidence of benefit. About 45% to 48% of treated dogs were judged as responding well, which was more than the improvement seen in the placebo groups (the placebo effect, contrary to what a lot of people believe, is common in veterinary patients and clinical research studies).
In a study done in Europe, only 17% of the placebo group showed an adequate response; considerably less than the 45% response in the Librela group. In a US study, however, the placebo response was about 36%, which is not nearly as different from the 48% response seen with Librela. Overall, the drug appeared to be effective based on the mechanism of action (biologic plausibility), the preclinical research in dogs, the response to similar drugs in humans, and the clinical studies done for Librela approval in several countries (Librela has been approved and used in many European countries since 2021)
The initial approval also included evaluations of safety. Studie in laboratory Beagles lasting form 2 weeks to 6 months were done at doses ranging from the usual clinical dose up to 10 times this amount, and no serious adverse effects were reported. Clinical dogs also reported few serious adverse effects compared with the placebo groups.
This is not, of course, a perfect or complete assessment of the possible risks of Librela. However, there is an inevitable compromise in the development of new medicines between the strength of the information produced to show safety and efficacy and the time, cost, and risk to study subjects needed to obtain that information.
A “perfect” study for determining safety would be to use the drug in thousands of dogs with arthritis, with all the complex mix of ages, breeds, medical conditions, and other treatments seen in the real world, for many years. However, this is impossible to achieve in most cases, due to logistics and cost, and requiring this would result in virtually no medicines ever being approved for use in veterinary patients.
The majority of drugs we have available in veterinary medicine are used those approved for humans and used “off-label” in our patients (see this post for a more detailed discussion of the drug approval process in veterinary medicine). We typically have a lot less information about the safety and effectiveness of these drugs than we originally had about Librela. So while the initial data were imperfect, it would be wrong to say that the approval was unusual or inappropriate.
Where We Are Now?
So what has changed? Since the US approval, there have been a lot of anecdotal reports to the FDA about bad things happening to dogs getting Librela. These have ranged from minor to severe, and they have included a tremendous variety of events. Some of the most concerning are neurologic changes and severe physical disability leading to euthanasia. This has raised the concern that some of these events may have been caused by the Librela.
Deciding whether this is actually the case or not, however, is quite a challenge. The majority of these adverse events have happened in older dogs, many of whom have medical conditions other than OA and are getting drugs or other medical treatments besides Librela. This is a population that is at high risk for all kinds of medical problems, including those we are hearing about. Determining what, if any, role Librela has in these issues isn’t as simple as just assuming any problem a dog getting Librela has is caused by the drug.
One thing the FDA has done to try and sort this out is something called disproportionality analysis. Essentially, they do statistical analysis to see if the reported problems are more common dogs getting Librela than in dogs getting other drugs, and they attempt to compare similar dogs based on age and other factors.
This is not a clear indicator that Librela is the cause, but it can raise the level of suspicion if there are a lot more instances of a particular problem than are seen in similar dogs getting other drugs. The FDA did find reason for concern in this analysis for several of the types of problems reported, inclduing some of the most serious.
The agency also looked at whether the reported problems were more common in dogs also using some other medical treatment along with Librela. Sometimes, this was the case, and they found that about 25% of the cases evaluated were also taking the medicine gabapentin. Again, this doesn’t show that there is truly a risk to combining these drugs, but it suggests this is a question that needs to be looked into.
Not surprisingly, the manufacturer, Zoetis, has tried to reassure vets and dog owners about the safety of Librela. In an email to vets, the company pointed out that despite the apparently large number of reports of adverse events, they are actually quite uncommon relative to the number of doses of the drug they have sold (the company cannot, of course, know how many doses have actually been given to how many dogs, but the sales figures are a rough estimate of this since vets don’t tend to keep a lot of unused drugs in stock). The estimated adverse event rate is less than 10 per 10,000 dogs treated by this estimate, though there is significant uncertainty behind this number.
It is also important to remember that people who have negative experiences with any drug are a lot more likely to tell others about it than those who have positive experiences, which is one of the reasons anecdotes are not a very reliable guide to the true safety of any treatment. In online discussion groups of veterinarians, there are often many anecdotes indicating vets have used the drug frequently without seeing any problems, and there are stories of dogs saved from euthanasia when they responded to Librela after failing other OA treatments. Dueling anecdotes often leaves us with more questions than answers.
We can try to make some sense of the limited data we have by looking at the way Librela works and experiences in other species. The drug reduces the amount of nerve growth factor (NGF). This is an important chemical with many roles in the body. Most critically, it is involved in development of the nervous system, which is why drugs like this should not be used in growing or pregnant animals. However, NGF is also part of the pathway that creates pain in OA, which is why reducing it can help control pain. It may also be involved in the maintenance and repair of nerve tissue and the bone and cartilage of the joints, so adverse effects regarding nerve function or bone and cartilage health might plausibly be related to the drug. However, there is not yet sufficient evidence for us to know if and when this is the case and which patients might be at greatest risk.
There has also been a lot of concern focused on the fact that similar drugs for reducing NGF have failed to be approved or have been restricted by the FDA due to concerns about adverse effects (e.g. 6, 7). The most serious problem was the development of Rapidly Progressive Osteoarthritis (RPOA), which can involve the dramatic and devastating collapse of joints. This has mostly been seen in humans taking both NSAIDs and an anti-NGF drug at the same time. It is not clear if RPOA happens in dogs or not.
While RPOA was not reported in the initial clinical studies, these involved fairly small numbers of dogs and the subjects were not allowed to take NSAIDs during the trial. Some vets have reported joint damage consistent with RPOA in dogs taking Librela, but again these haphazard case reports are not yet sufficient to know when, if, and in which dogs this problem might occur.
As always, we have to bear in mind that humans and dogs share a lot of aspects of our biology, but there are also important differences that affect how we handle drugs. Humans can chew sugarless gum with xylitol safety while this chemical easily kills dogs. Dogs can take the antibiotic enrofloxacin routinely while humans get unpleasant hallucinations from it. The evidence in humans is worth paying attention to, and it can be a clue to what might be happening in dogs, but it is not sufficient proof in itself to make a confident judgement.
What Do I Do?
The frustrating reality is that right now we don’t have a firm, final answer to how risky Librela is for each patient. The best we can do is integrate what we know with the level of uncertainty and the needs of each individual patient and make a choice now, knowing that our decision might be different in the future when there is more, better information.
Though I am involved in canine aging research, and I have even worked a bit on osteoarthritis, in my clinical practice I mostly see emergency and surgical patients, so I haven’t used much Librela myself. Many of my colleagues in the practice have used it, and anecdotally they have seen mostly positive results and few of the concerning adverse effects discussed here.
My own approach, then, is based not so much on anecdote or personal experience but on my analysis of the evidence and uncertainty at this moment. My judgement will certainly change as new information comes in, which is, after all, the whole point of evidence based medicine. For now, here’s what I tell my clients and colleagues-
- Like all drugs, Librela has both risks and benefits
There is reasonable but limited evidence for beneficial effects on OA pain, though the response rates in the published studies are less than 50%, and this may include 15%-30% placebo effects. I think it is appropriate to use for OA pain with the caveats below.
- While the risks appear quite low based on studies for approval, there are a lot of reports of more serious issues now that it is on the market. We don’t know for sure if these are actual problems with the drug, but they might be.
Anyone who says Librela is absolutely killing and disabling dogs in droves is going well beyond the data. Anyone who says Librela is a clearly safe, first-line OA drug with minimal side-effects is also going beyond the data. The uncertainty about the real risks and the factors that determine which dogs can safely use it and which can’t is enormous at this time. Because of this,
- Librela should not be the first thing we try for OA treatment.
We know a lot more about the safety and benefits of some other treatments. NSAIDs are the best first-line drug treatment, and the fears about them are excessive, irrational, and quite likely part of the reason we may have jumped too early and enthusiastically to using Librela. Some dogs truly cannot use NSAIDs due to other conditions or medications, but I routinely see dogs who could benefit from these drugs not using them because of unreasonable anxiety on the part of vets and dog owners.
There also other therapies for OA with decent supporting evidence, including weight loss and a few supplements (e.g. fish oils, green-lipped muscle). Rehabilitation (aka physical therapy) is a plausible and promising option, though we have little data as yet about what works for what cases.
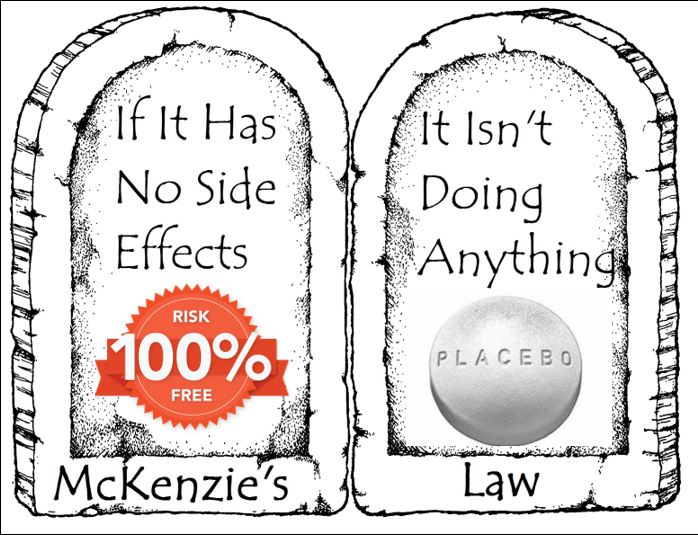
There are also lots of implausible, unproven, or useless therapies out there, from CBD to glucosamine, acupuncture to cold laser, tramadol to gabapentin. While most of these are likely to have minimal risks, they don’t have strong evidence that they work either. If we use the current concern over Librela to justify greater use of such treatments, we will very likely be leaving a lot of dogs with inadequate pain control. It is also worth remembering the basic priciple of biology that there are no benefits without risks. Or, as I like to call it, McKenzie’s Law:
- In dogs that can’t use NSAIDs or other treatments with good supporting evidence, or dogs who aren’t sufficiently comfortable on these, Librela can be effective and even life-saving. I think it is worth trying in these cases, with appropriate discussion of the potential risks and the uncertainty around these, and with proper monitoring.
- Librela should probably not be given along with NSAIDs.
We don’t yet know if dogs will have the same issue of rapid cartilage destruction seen in humans. Some cases that look like this condition have been reported, but it’s too soon to know if/when/how often/to whom this happens. Most of the dogs who could safely use NSAIDs probably won’t need Librela anyway, but this limitation seems prudent right now.
Some specialists recommend x-rays of joints before and regularly during use to watch for signs of cartilage destruction. This might increase safety, but it can be expensive and may need repeated sedation, so not always practical.
- Librela probably shouldn’t be used in dogs with neurological symptoms, such as weakness or incoordination (aka ataxia). Partly this is because it won’t help if they don’t have pain or OA anyway, and a lot of the time hind limb weakness in of large-breed older dogs is due to neuromuscular disease rather than OA. However, this might also be a group at higher risk of adverse neurological effects based on both the reported adverse effects and the mechanism of action of the drug.
- I recommend regular recheck visits to look for any problems in dogs taking Librela.
I would typically recommend and exam 1 month after first dose and then ever three months for at least a few visits, and x-rays of any joints that seem to be getting worse. This is a pretty arbitrary schedule, and other approaches are also reasonable, but this level of monitoring also isn’t a bad idea for dogs with chronic musculoskeletal issues anyway, especially if we are trialing multiple treatments.
I also recommend the use of objective tools for measuring pain and disability, such as a validated pain scale or mobility tool. Placebo effects influence owners and vets alike, and these can make ineffective treatments look like they work.
Bottom Line
- Librela is likely mildly to moderately effective for OA pain, though we do not yet know which dogs will respond best and for how long.
- Librela has risks as well as benefits, but we don’t really know how common these are. We also cannot predict very accurately which dogs are most likely to have adverse effects.
- Librela should not be used in dogs with neurologic disease or taking NSAIDs
- Librela should not be the first choice for most dogs with OA (weight management and NSAIDS are the best first-line for many dogs, and there are other options with some supporting evidence if these are not possible or sufficient).
- Dogs on Librela should be closely monitored on a regular basis
Things will change. As more information is produced, we will have a better sense of how well Librela works, what the risks are, and which dogs are more or less likely to experience both benefits and risks. My hope is that we will be cautious but not hysterical in our use of this drug while more research is done. We don’t want to cause harm, but we also don’t want to abandon a potentially useful treatment without sufficient cause.










Thank you so much. I have an 8 year old Collie who is beginning to show some signs of arthritis. I hope you will continue to follow and report on Liberal
I currently use this medication for my 15 year old Labrador. This was our last hope. I understand there are risks and benefits to everything that we do everything that we take. October 2024 I would’ve euthanized my dog had this medication not started helping. It is now January 2025. I have a dog that now has 75% of her mobility back and doing quite well. This medication has been very effective with my dog. I know some cases it may not be, but our case has been successful.
I run a Librela group myself, but with data on the dog (age, weight, dose, diagnostics, therapies, medication,…) and factual experience reports.
Many people let their dogs play and jump regardless of the disease and then report ataxia, cruciate ligament ruptures etc. This seems to me to be a major problem and I think Zoetis’ back-to-play plan should be communicated much more clearly. Only in a few patients was there no reasonable explanation for the ataxia.
Polydipsia, polyuria, incontinence, restlessness and lethargy are reported more frequently. In my opinion, the likelihood of this is also high, as they usually occurred with the injection and later subsided or disappeared after discontinuation. Overall, however, they are rare.
A good approach might also be to compare the general occurrence of illnesses/symptoms in dogs with the reports. For example, how common is pancreatitis in general and how common with the drug.
Insurance companies should have the data on this.
Finally, it should also be borne in mind that drugs for which there are groups in the social media are more frequently reported negatively. See Bravecto and similar
Sadly, basic epidemiological data, such as the prevalence of common conditions, is often lacking, and it is especially complex because of the great variability between breeds, so comparisons like you suggest are useful but often hard to make.
I do think that more clinical studies are going to be needed, both retrospective and ideally prospective, to sort out key risk factors for negative outcomes as well as variables that might predict a good response. I am hoping these get done. Since the drug has been in use for several years in Europe already, there may already be some data that could be used for at least preliminary retrospective case/control studies.
And yes, you are absolutely right that while almost all drugs get blamed for bad things once they are released, especially if they are wisely used, those with higher media profiles do draw more negative responses. With Librela, a lot of the reports have come from vets, who might be a little less likely to overreport based on media attention, but it’s still an issue.
Thank you for your balanced piece on this important topic. Have you any thoughts/insights on NV-01/ranevetmab, the predecessor canine anti-NGF mAb that quietly fell by the wayside (while the feline version NV-02/frunevetmab proceeded)? It’s my understanding that an investigational new animal drug file was opened with the FDA CVM for NV-01/ranevetmab circa 2012, registration studies were carried out in hundreds of dogs (I believe more dogs were treated on studies with research grade NV-01/ranevetmab than with research grade Librela/bedinvetmab), and it was targeting FDA approval circa 2016. Then NexVet was acquired by Zoetis, and Librela/bedinvetmab moved forward. Very little information has been released to the public about the NV-01/ranevetmab clinical trial data, and I feel like some of it was conflated with Librela/bedinvetmab. I sure wish we knew more about these patients, especially their long-term followup.
Interesting. I am not familiar with that agent, and I haven’t seen any of th related data. It is, unfortunately, all too common for study data from products that don’t make it to market to be archived and not published,d which is a huge loss. This was the target of the AllTrials initiative a few years ago, though that seems to have petered out.
In an attempt to increase mobility in my 16 year old rat terrier I decided to try the Librela injections beginning of Sept. Was told by my vet about the drug and there were no side effects. My dog did have other issues as you would expect in one this age and was using accupuncture/ laser for pain relief as well as gaba and amantadine. Saw improvement so proceeded to second injection Oct 4. Four days later she had a seizure, never had seizures before this. No better improvement in mobility. One more injection 10/31 and decided if still no improvement I would discontinue as I did not want excessive drugs in her body if not helping her. Month of November was rapid decline in mobility, diarrhea for no reason, confusion, staring into space, getting stuck under furniture, developed skin infection mostly on her front legs but also a spot on side of her face and samples were taken at vet on 12/12 to determine treatment. Results would take 10 days. Finally noticed blisters on her lips as well by 12/14 and could not support herself on hind end at all swaying from side to side then dropping down to lay on her side. By 12/15 and 12/16 seizures caused further decline with the last one causing the most damage. She was in hospice care since 12/14 by her vet. I made the heartbreaking decision on 12/16 to euthanize her as she did not recover that day. This was when all of the news stories/warnings came day after day across the country. Until then I never considered that Librela was the reason for her rapid decline. I never had a dog live this long and thought this was all a normal part of her aging. I had no reason to research it as my vet did not suggest a connection. Hearing and reading others experiences convinced me the similarities all pointed to Librela. It’s too late for my Cocoa but she did not deserve to suffer this way in the end. All of her symptoms were being controlled with other treatment up until Librela. I thought I was doing the right thing at the time to help her just a bit more but would NEVER have tried Librela if I was made aware of the devastating side effects. I feel pet parents should make their own decision regarding their precious dogs however the warnings should be FULLY revealed to them in order to make the decision. After all of the negativity surrounding this drug now whether or not it is Librela anyone considering this treatment needs to be educated by their vet. We should not have to research on our own when our trusted vet is recommending a treatment, we trust them. I believe however we were (including vets) misled by the manufacturer as well as the sales reps. Please help prevent unnecessary damage to our precious senior dogs.
Hi My fox terrier dog had bersansa 4 times and now can not walk her ligaments and joints have failed she has had a joint tap i get results today she has splints on 4 legs ans she never had a problem until having the beransa , one vet wanted to put her down Tara my dog may have to have surgery now carpal arthrodesis to save her legs so she can walk again . I am so upset and regret allowing the vet to give her Beransa it never should of been a first option .
I intend to contact the company and possibly take legal action my dog is 7 years old .
Lisa
More anecdotes… Sophy (papillon, now 16) has been on Librela for a year. She reacts badly to NSAIDs and had previously been taking a carefully measured dose of paracetamol for pain relief. It took a couple of months on Librela to see an improvement but it was then very definite – she will often run short zoomies while out on walks, and is significantly more comfortable and less restless in the weeks after the jab while sometimes needing pain relief in the last few days before the next one. She can be a bit wobbly when first standing or on uneven surfaces, but then she was getting that way before the Librela. She definitely drinks and pees more – she had full blood tests before a recent dental and everything was spot on normal with no indications of kidney or other issues that might cause polydipsia or polyuria, so I think these are probably caused by the Librela. I did research the possible side effects and discussed them with her vet before starting her on it (I had some concerns about the time it would take to clear her system should she have an adverse reaction), but given her age we are both firmly of the belief that quality of life is more important than longevity at this stage. The monthly Librela injection is always given by a vet, so she is checked very regularly.
I note with interest your comments on not combining Librela with NSAIDs – I had been planning on trying Galliprant as Sophy reacted badly to meloxicom several years ago, but may hold off on that for now. Paracetamol is not ideal – I have a cat as well as the dogs, and have already had one expensive and nerve wracking dash to the emergency vet when she got into Sophy’s paracetamol-laced food – but as occasional top up pain relief it is manageable. Weighing up the known risks and benefits this seems to be the best balance for us at the moment.
Are there similar concerns for Solensia in cats?
A lot fewer reports have been raised about solensia, though there are some (as for any drug). The most common is itchy skin and a rash, often on the face, which resolves with stopping the medication. You can find more safety information in the evidence summaries from the European and U.S. licensing for this product. There is also a summary of adverse events reported to the FDA though there is no evidence to determine whether or not these were really related to the drug or not.
I was in the process of deciding when I was going to let my 14 1/2 yr old lab/boxer/gold ret mix go because he couldn’t get up 1 step without falling backwards, his hindquarters would give out when he was eating and his front legs started to fail when he was drinking water, and was in general having significant mobility issues.
My vet recommended a new drug, Librela, that had good results in some dogs but not all dogs. Within 3 days of his first injection he was walking up steps and around the house and yard with no issues. We were able to go out for walks again, he interacted with my other dog once more, and he stopped falling when eating or drinking.
He got a monthly injection for 7 months until it was time to let him go.
I did try this for my other 9 1/2 yr old dog who has hindquarter issues but didn’t see any mobility improvement after 3 injections, so stopped using Librela.
Our dog died 8 days after a librela shot. She suffered a sezure and never came out of it, and had to be put down. Say what you want a out study this and study that, but everyone i know that has given this shot to their pet has had to mourn the loss of their pet.
Has anyone looked into the necropsy reports on the previously young, healthy Beagles, 17-18 months old at end of the 6 month trial? I’m not a vet but it seems that a lot of internal damage is being seen in many organs. Is this a safe option for any dog? A vets interpretation of this would be helpful for people thinking about using Librela. https://www2.zoetis.com.br/content/_assets/%5bMGR%5d-Animais-de-Companhia/%5bMGR%5d-deZenvolve/%5bMGR%5d-Especialidades/PDFs/librela-krautmann-laboratory-safety-evaluation-of-bedinvetmab-a-canine-anti-nerve-growth-factor-monoclonal-antibody-in-dogs.pdf
Yes, necropsies are required for most safety studies used in drug approval. The results are available in the FOI report.
Of course, this is tragic whether or not it was caused by the Librela. But thousands of people have also reported being able to delay euthanasia and enjoy more time with their dogs due to using this drug, so stories are used to argue both sides of this. That’s why studies are needed.
This paragraph was removed from a lot of Librela information in different Countries somewhere around 2022 + 2024. Luckily, it’s still on this Canadian information document. Could this be a link to RPOA? Could it have been removed because some orthopaedic specialists were joining the dots? “Of the 89 dogs enrolled in the 6 month open label EU continuation study without a placebo group, three dogs, aged 13, 15 and 16 years were diagnosed with Leydig cell tumors; 1 dog had a fractured coronoid process and another dog had a supracondylar fracture and there were two dogs with mild or moderate proprioceptive deficits not considered to be related to osteoarthritis. The causality for these events was not determined.” As far as I’m aware, all dogs were screened before the trials. https://www.drugs.com/vet/librela-15-mg-can.html
My collie’s hocks both collapsed while on Librela and metacam, which I was persuaded to give on top of the Librela when Librela as he continued to deteriorate. He’s now has surgery to repair both hind legs and he’s on no pain meds at all – just passive range of movement exercises, massage and hydrotherapy swimming, and he’s happier and moves better than when in the pain meds (which he’s off because he developed a grade 2 heart murmur and bio markers for kidney and liver problems while he was on them). There is good, objectively assessed evidence for physical therapies relieving pain and slowing arthritis – better I would say than the short term trials of the pain meds in dogs. Unfortunately, though, there isn’t the funding for so many trials of physical therapies as for the drugs.
We had a horrible experience with Librela. Was told it was a miracle drug. Our poor girl suffered tremendously. She was 8 certainly not old, had a perfect checkup. Had never been on any arthritis meds. Panting, excessive thirst, diarrhea, ataxia, lethargic, whining, hiding, nose
Bleeds are just some of her side effects. The risks certainly were not worth the agony she suffered. Six weeks of suffering and she did not survive. Never again will another dog of ours be injected with Librela.
Thank you skeptvet for a balanced view! I’m sorry, I replied in too much of a hurry to Cynthia, thinking I so wish I was back in her position, ie with what I would think of as a fairly young collie with the first signs of arthritis. Mine was 9 when he was started on Librela, a very lively and active dog. I wish I had known then what I know now about Librela, the human trials of the human version, the reliance on subjective assessments of pain (by owners) in the trials of NSAIDs and Librela in dogs, and that although these pain meds are being prescribed by vets long term, they have not been trialled in dogs long term, and the post-authorisation pharmocovigilence seems to be all over the place, with a lot of underreporting, and assessments based on averse events per dose rather than per animal treated. The human trials of the human version of Librela (which were massive in comparison with the Librela trials) seem to have demonstrated significantly higher incidences of rapid joint degeneration in patients who had received more than three doses. My dog suffered bilateral tarsal-metatarsal luxation between his 15th and 18th doses of Librela, and the vets had not spotted anything wrong with those joints before then. I also wish I had known back when my dog was first prescribed Librela, that, as the vet pain specialists seem now to acknowledge (see for example the COAST guidelines 2023), physical therapies and an appropriate exercise regime, preferably planned by a qualified physiotherapist, should be put in place first, before resort to pain meds. There is what seems to me to be good evidence of the benefits of physical therapies in dogs, based on objective measures. I can send you references if you would like them.
My dog ??died ten days after his one and only injection. This is what he experienced in his last days of life: excessive thirst, vomiting bile for an entire night, loss of appetite, paralysis of all four legs, and sudden death with cries of distress as he died and stiffness. All this in two days. A night I will never forget. A choice I will regret for the rest of my life.
if your interested the chatbot hard to find librela nsaid study showing one nsaid not sold by the company making librela does not work any better than librela. see the link below. I use the nsaid made by the company that makes librela so i wish the company had used there own nsaid in the study. I wonder why they did not use their own. see https://x.com/i/grok/share/4O4yE6asHj2gvHXcA8FONxL7H
My dog had to be euthanised after two injections, she slowly died in front of my eyes, but because I was told there were no side effects (and yes I read the leaflet which said they only side effects noted at the time in the UK were increase drinking and urination) I did not put two and two together and allowed the second shot, arguably the damage was already done, we will never know. After the second shot, in the space of two weeks, her mobility declined to the point she could no longer stand, she was barely able to sit up, she drank excessive amounts of water, she developed a cough, heavy breathing, howled in pain while suffering a seizure, lost cognitive function (would gaze into space) became more nervous, she would not sleep, refused to eat, her muscle wasted alarmingly quickly, her nose and gums were bleeding, we could not ask her to go on, we put her into the boot of the car and she had one final road trip to the vet where we said good night. Librela took my girl before her time, I will never stop fighting for tighter regulation of its use.
My 7yr old GSD had 2x librela for mild arthritis..her side effects included panting, restlessness, aggression toward our other dog followed by excessive drinking, peeing and voracious appetite and opaque thick drool followed by several weeks of urgent diarrhea.
Now at 180 days post librela she seems back to normal..( I hope )
The same thing happened to my Bull Terrier. Librela and Metacam. Aged 8.