One of the most common topics over the lifetime of this blog has been treatments for osteoarthritis in dogs and cats. I’ve talked about pharmaceuticals, acupuncture, electromagnetic fields, laser, and other treatments, but the bulk of the articles have addressed the most popular over-the-counter (OTC) remedies for this condition, dietary supplements.
Supplements are ubiquitous, recommended by vets and used by owners frequently despite scientific evidence that is inconclusive or that outright shows they don’t work. Over the time I have been covering this topic, science-based medicine has provided new tools for treating arthritis, such as the use of monoclonal antibodies to reduce pain and inflammation in dogs and cats. For most pets, non-steroidal anti-inflammatory medications (NSAIDs) also remain a safe and effective treatment. There are also promising approaches, such as CBD and physical therapy, that have some encouraging supportive evidence, though more research is certainly needed for these. Despite this, pet owners, and even vets, have a tendency to stick with outdated OTC remedies that are unproven or even clearly ineffective.
The paragon for this is glucosamine/chondroitin. I wrote about the poor evidence supporting use of this supplement in arthritis pets in the very first month of this blog, June, 2009. At that time, I stated-
There is virtually no good quality research on the use of glucosamine and chondroitin in veterinary patients. The best study so far, done in dogs, found a combination of these agents to be of no benefit for patients with osteoarthritis. Further research in animals with osteoarthritis is warranted, but at this time the evidence does not support the use of glucosamine and chondroitin in these patients.
Since then, the negative evidence has piled up, in humans and in animals. My most recent summary in 2020 concluded-
The failure to find consistent and compelling evidence of clinically meaningful benefits after decades of extensive research strongly suggests such benefits are negligible or nonexistent.
Despite the seemingly minimal impact of such consistently negative findings on pet owner behavior, I feel obliged to continue to review the evidence and encourage both vets and owners to use therapies with real evidence of safety and benefit whenever possible. A recent systematic review (the highest level of evidence available) has once again looked at glucosamine, along with a host of other diets and dietary supplements for arthritis in dogs and cats, and hopefully their findings will shift the zeitgeist a bit on how we manage this condition.
Barbeau-Grégoire M, Otis C, Cournoyer A, Moreau M, Lussier B, Troncy E. A 2022 Systematic Review and Meta-Analysis of Enriched Therapeutic Diets and Nutraceuticals in Canine and Feline Osteoarthritis. Int J Mol Sci. 2022 Sep 8;23(18):10384.
The figure below illustrates the quality of evidence for five categories of potential therapies. The proportion of studies showing the highest level of evidence, an effect compared with a placebo (Effect), an intermediate level of support, improvement over time without such a comparison (Improvement), or no effect at all (Non-effect) are shown.
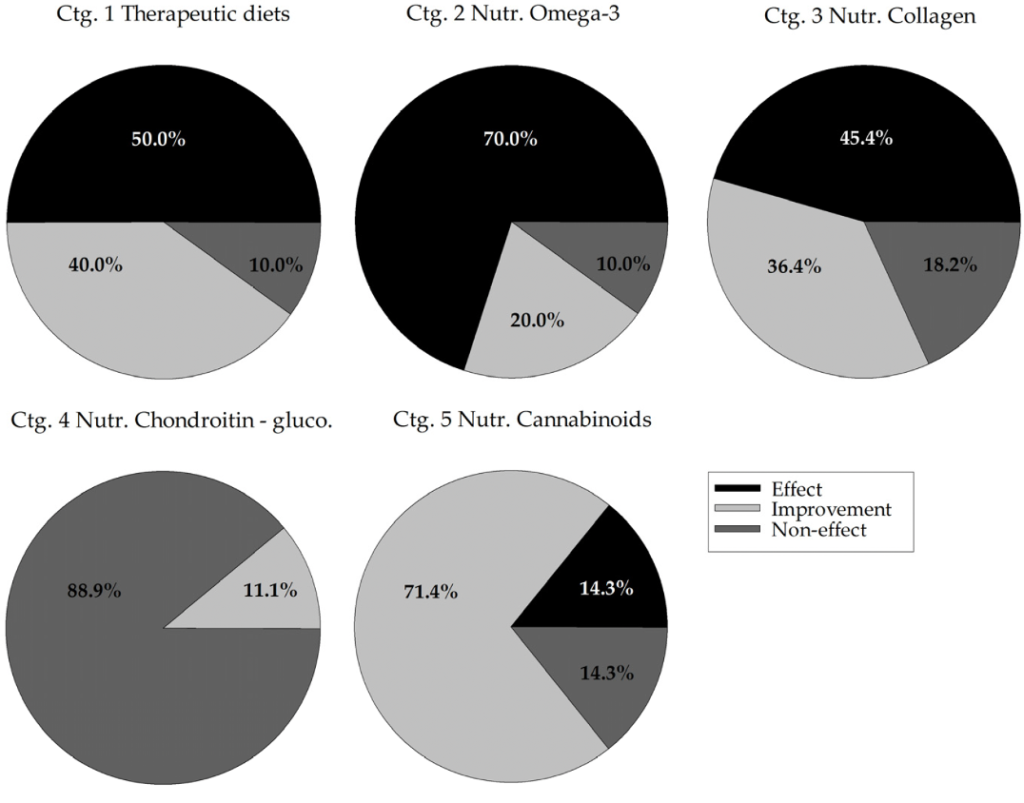
The authors also evaluated the number and methodological quality of the research showing these effects and provided conclusions on each intervention. Here are those conclusions-
- This meta-analysis supports the use of omega-3 supplementation for the management of canine and feline OA.
- The results of this meta-analysis [for cannabis] are promising, but further investigation is needed to determine the efficacy, doses, formulations and combinations recommended for the treatment of canine OA pain. Further studies will also be necessary to conclude on the use of cannabinoids in cats since none have been carried out to this day.
- It, therefore, appears impossible to rule, at the present time, on an indication for collagen in canine OA based on the results of this meta-analysis.
- Like these previous reviews, the results of the present meta-analysis led to the conclusion that chondroitin-glucosamine nutraceuticals should not be prescribed in canine or feline OA.
- All the other nutraceuticals evaluated did not present sufficient evidence of efficacy to decide on their indication.
I am not naïve enough to imagine that this will lead to a widespread abandonment of glucosamine, but I hope that the consistent buildup of evidence over decades showing that this is an ineffective treatment, and the active recommendations against it by experts in both human and veterinary medicine, will at least discourage the substitution of this failed approach for treatments with much better evidence for real effects.










I stopped using chondoitin & glucosamine because of that 2009 article. I had been doubtful the supplements were having any effect before reading the article, so it was easy to accept as it confirrmed my own observations. I struggled more with raw feeeding, but gave that up too eventually. So thank you for helping me make those changes.
Pingback: Evidence Update- A Systematic Review of Diets & Dietary Supplements for Arthritis in Dogs and Cats (TL;DR- Can we please stop giving them glucosamine?!) - Herbs 2 Healing
Thank you so much for this in-depth review!
I was wondering if you had an opinion on Solensia, the novel monoclonal antibody treatment for feline osteoarthritis pain. Or if you could comment on the logic of my own analysis.
My vet recommended it, but after checking Solensia’s own website for veterinarians (plus FDA and EU announcements), I am skeptical. I am not sure how this site handles links but it’s at I am not sure how this site handles links but it’s at solensiavetteam dot com
My background is social science but with interest in quantitative evaluation, an MSc degree.
Solensia’s claim to fame comes from a clinical trial with 275 otherwise healthy cats with clinical signs of osteoarthritis in at least two joints or spinal segments, which showed pain. They state that 77% of participants showed improvement in pain over 12 weeks (defined as reduction of at least 2 points in the total CSOM score – Client-Specific Outcome Measures – and no increase in any individual score, on a scale of 3-15). They also claim 12.9% improvement in mobility symptoms after just 3 weeks – looks like using an objective measure of activity count per minute.
BUT! Not only did 68% of participants in the placebo group show the same improvement by the end of 12 weeks (and the improvement lines are somewhat parallel-ish). For mobility, if you actually look at their entire graph, all symptom improvement started to decrease around week 7-8 and was completely gone by the end of 12 weeks (and there was no improvement at all in the placebo group, highlighting the difference between the results of the objective and subjective measures).
Basically, the way I am reading it, Solensia actually flopped on their own objective measures. And the “breakthrough” improvement was shown on subjective measures only, where placebo effects alone led to 68% of owners reporting improvement at the end of 12 weeks. I also noticed that instead of featuring mean CSOM score changes, they are reporting percent of owners who found improvement as defined (at least 2 points change). My take on that is that the magnitude of improvement was probably not impressive enough – otherwise they would have used it.
In humans, self-reports for pain and placebo effects can carry a lot of validity and clinical meaning because pain is so subjective. For myself for example, I would be ok taking glucosamine/chondroitin because it’s cheap, seems to have no harm, and there is a chance to benefit from placebo effects.
But in animals, placebo effects seem to be more about owner’s attention and optimism? Especially, when the magnitude of reported change is most likely small and the results of the objective measures differ so much from the results of the subjective ones? Basically, to me, these results indicate that the true breakthrough of Solensia is more in marketing…
Anyway, I would deeply appreciate if you had a comment but also completely understand if that’s too much to ask.
All good questions and observations!
I think the core difficulty here is assessing pain and response to analgesics in cats. We really have no effective objective assessments, and the subjective tools all have pros and cons and significant limitations. On top of that, of course, there is a large caregiver placebo effect. Therefore, there is always going to be some significant uncertainty about the effects of pain relief interventions.
Anti-NGF monoclonal antibodies have a plausible mechanism of action, and there is good evidence in lab animals and in humans of benefits, so that informs our interpretation of clinical trial events somewhat. I’m not sure which document you’re using to get the data, since there are a number available, including-
Solensia insert
Solensia FOI Summary
Pilot study report
Pivotal efficacy study report
These all report the same data in slightly different ways.
My takeaway from these is that the frunevetmab groups typically showed a higher level of perceived improvement on the CSOM and owner global assessment measures, though this was not statistically significant at all points. In the pilot study, there was also an FMPI assessment, which generally did not show convincing differences between groups, and accelerometry data which were pretty difficulty to interpret in a cogent way. Both studies also had a subjective veterinarian exam measure, and this showed no difference in the pilot study but did show an effect of the treatment at a couple of timepoints in the larger field study.
Overall, I think the evidence is reasonably consistent with some benefit, though how consistent, how large, and how lasting are unclear. Given the difficulty in assessing pain in cats and the limited options we currently have for treating OA pain (mostly NSAIDs, which unfortunately many owners are reluctant to use and which legitimately can’t be used in some cats), I think it is reasonable to try this treatment if other measures, particularly weight loss and NSAIDs, are not possible or have failed.
I using started using chondoitin & glucosamine because the drug salesmen selling it came to me about 30 years ago with pictures of xrays showing before and after dog joints clearing of arthritis when treated with these quackery drugs . Did not need a randomized controlled trial i though because i could see for myself the arthritis go away on the xrays. I am sure all those guys showing us the bogus xrays up the supply chain are retired sipping on a pina colada on some island laughing.. The government had to spend millions to prove it does not work so everyone got taken even if you never bought it.
still searching for link to support my post that fed gov had to spend millions of dollars to debunk these gag drugs. chatgpt could not find anything for me. My point was it cost the federal government money to debunk quackery so why let people sell unproven medical care in the market place from the get go without proving it works. When the govenment let them sell unproven medical care in the market place without spending their money to do testing the government ends up spending funds to debunk it.
Pingback: Are the 10 Best Supplements for Senior Collies/Dogs Safe?
Since this study was only regarding analgesic effects of glucosamine-chondroitin, does that conclusion move towards supporting that it’s also non-effective in using it as a supplement for dogs and cats that are prone to OE? Munchkin cats, GSDs, etc, for example.
It’s interesting to realize that owners are thinking that this supplement is meant to help the pain! I’ve always heard it explained as something to be used in conjunction with NSAIDs or other treatment. Clearly there’s been a breakdown of communication in every direction about what this supplement is supposed to do… Thanks for the post! I’m excited to discuss this at work with the vets and other techs, lol.
As a side note, I couldn’t find anything about Adequan on your blog. It’d be interesting to hear what you think regarding Adequan, especially since I’ve seen my own pets do well with it.
These supplements are also promoted as “chondroprotective,” but the evidence is no better for that. We can always posit that each time the evidence fails to support one possible benefit there may be another we haven’t looked closely enough at, but realistically decades of use and research have come up with almost nothing beyond anecdotal support, and that’s a pretty bad sign for any therapy.
I keep meaning to do a post on Adequate, but never seem to get around to it. Thanks for putting it back on my radar!
Thanks for the update. I was searching for any updates on the state of glucosamine as an arthritis med for dogs, since I remembered it being recommended by one of my vets many years ago. At that time, I looked for evidence on my own and read a number of studies, none of which showed any observable improvement. Now my 13.5-year-old 74-pound cattle dog takes gabapentin twice a day. I’m curious about adding marine-based oils, but don’t want to add anything for which there isn’t good evidence.
The evidence for fish oils as an arthritis treatment in dogs and cats is generally encouraging but pretty limited. Given the low risk, I think they are reasonable to use so long as other therapies with proven benefit (such as NSAIDs) aren’t avoided when they are needed.
The most recent systematic review covering the subject concludes:
“[Despite some risk of bias in the studies]. in general terms, there is sufficient evidence to consider the benefit of long-chain omega-3 fatty acids, such as EPA and DHA, as adjunctive therapy in canine and feline patients diagnosed with osteoarthritis.”
*I promise, this is NOT hate mail disguised as admiration*
I think this site is amazing! When I first stumbled upon you years ago (by seeing how many comments you delivered to and respect of you by Linda P. Case’s blog), I was so…entranced! I think I read your entire site of blogs in two days (I skipped all of the comments after realizing many were quite…angry).
Am I correct in assuming that anecdotal evidence, when there is enough of it, is one of many items that can prompt scientific studies? I may be wrong, but I have yet to read any scientific studies regarding “Just in! New scientific study reveals that there is, in fact, ZERO correlation between feeding your dog/cat cigarette butts (with or without tobacco removal) and extended length of life”. And yes, that was snarky sounding, but it was the most bizarre item to come to mind.
Now, to that, let me add that I do pay attention to user experience/anecdotal evidence. If I read about a product or type of product that is seemingly addressing one type of malady or another (that is also problematic to one, or more, of my boys), I will do further searching. If my searching pans out decent (ie I think I might like to give it a go), I then search for REsearch (I know the difference between searching and researching). If this fails to show benefits, yet also determines it is not harmful, I will usually give it a go and do my own anecdotal observations. Regardless of whether I see great benefit or none (as long as I see no harm), I would never recommend the product (or product type) to others unless I were specifically asked. Even then, I would be careful with my words, suggest they do their OWN searching and REsearching, before using said product (or product type).
This is my theory for a few reasons, but mainly because…science changes. I do not recall the exact year, but at one time this website stated (paraphrasing here) ‘CBD oil has no clinical evidence for effectiveness for dog/cat osteoarthritis or other physical pain’. This stance has changed since the original mention. I would be ill-at-ease knowing I withheld possibly helpful, not harmful, intervention to assist my pet with pain (or any other ailment) simply because of lack of clinical studies in peer reviewed journals.
I also beleive every dog/cat is different. What may work for MY boys, quite possibly will show no effect on others, anecdotal or not. Good example is Proin. This was not useful for one of my boys that is like an old faucet…drip…drip…drip. It was effective for one of my foster dogs, results apparent in just 3 days. And there is plenty of clinical studies on Proin. You may, or may not, be interested to know I then searched for other, less pharmaceutical methods…marshmallow root, dandelion root/leaves, echinacea parts etc. and found none of these helpful either. So far, my most promising results have been with a human sized bed pad covered with a highly absorbent, thick cotton towel on my bed (he is a big boy at +/-70#. This is true leakage, not full-on, empty the bladder urination.
I do not believe you have ever argued that anecdotal evidence is useless, so I am not inferring that is your stance.
To all of this, I would like to add that I find it incredibly noble that you and your team have decided to tackle gerotherapeutics in our canine companions, similar to Dr. Peter Attia in humans. I find this highly respectable and a very welcome addition to the canine scientific world. Than you so much.
Paws Up !
SonJa
“Am I correct in assuming that anecdotal evidence, when there is enough of it, is one of many items that can prompt scientific studies?”
Absolutely! The main value of anecdotes is to suggest hypotheses to test. Sometimes these turn out to be correct, sometimes not, but the anecdote serves to prompt investigation, not to prove the idea one way or the other.
“I have yet to read any scientific studies regarding “Just in! New scientific study reveals that there is, in fact, ZERO correlation between feeding your dog/cat cigarette butts (with or without tobacco removal) and extended length of life”. ”
What you have hit on here is the concept of biologic plausibility. not every idea is reasonable, and scientific studies are only worthwhile when an idea is reasonable. Scientific research into homeopathy, coffee enemas, the power of magical methods like Reiki, or the feeding of cigarette butts to dogs and cats make no sense because for the hypotheses being tested to be true, a lot of well-established science that works in many other areas would have to be wrong. That’s not impossible, and once in a great while a far-out idea is actually correct, but most often claims that overturn previously well-established knowledge don’t turn out to be true.
“I do pay attention to user experience/anecdotal evidence”
You are mixing different situations. User experience info can be useful for giving a sense of how other people have experiences something you are considering using. It can’t prove that their experience is the same you would have, nor that their beliefs about the experience are true, but it may still help you to make a decision. If everyone likes a new movie,. it is reasonable to think. about going to see it, though that doesn’t guarantee you will like it.
This is a bit different from anecdotes being used to guide medical decision making. There is no right or wrong about whether a movie is any good, but there is an objective right or wrong answer about whether a medical practice can effectively treat a disease, and science will get us a lot closer to the truth of that than anecdotes.
“science changes.”
Absolutely! But this is not a sign of its unreliability, it is a built-in feature. One of the reasons science is so much more reliable than tradition or experience is that it changes as the evidence changes. Mainstream medicine used the dangerous and ineffective practices of bloodletting for thousands of years, and then eventually gave it up when science showed it did more harm than good. Traditional Chinese Medicine and homeopathy, on the other hand, continue to rely on the same ideas and practices despite the evidence that has accumulated showing they don’t and can’t be true. Science isn’t always right, and the understanding we have now will change, but over time and on balance, it gets us to the right answers more often than the alternatives.
” ‘CBD oil has no clinical evidence for effectiveness for dog/cat osteoarthritis or other physical pain’. This stance has changed since the original mention. I would be ill-at-ease knowing I withheld possibly helpful, not harmful, intervention to assist my pet with pain (or any other ailment) simply because of lack of clinical studies in peer reviewed journals.”
First, the statement that “there is no evidence” does not mean “this doesn’t work.” It simply means we can’t say whether or not it works until there is evidence, and that we can only be as confident in our judgement as the strength of the evidence justifies. In this case, evidence developed that there may be some benefit. But if you had chosen to use the treatment rather than wait for the evidence, you could just as easily have made the wrong choice if the evidence had gone the other way. If it had turned out CBD caused liver failure, for example, waiting would have been the right thing to do.
The problem is that people look at cases where a new idea proved correct and think “Oh, well I should have accepted that before the scientific evidence was in.” They never seem to look at the far more numerous new ideas that don’t prove true and think, “Oh, I shouldn’t have sued that until the scientific evidence was in,” or “Good thing I waited.” All of the millions of dollars spent on glucosamine, resveratrol, and many other products I’ve reviewed on this site which have turned out not be helpful could have been better spent if people had followed the science, not anecdotes. So while the final verdict on anything can’t be known in advance, waiting to decide until there is good evidence one way or another is the safest bet.
“I also beleive every dog/cat is different. ”
Ture, but this doesn’t mean that anecdotes tell us what works for any given dog. Lots of people will tell you that faith healing, magic rituals, worthless supplements, homeopath, etc. has “worked” for their dog, but because anecdotes only focus on the one possible cause that the person is thinking about, and ignore all the other variables, they don’t reliably separate human bias from what actually happened. They may seem like they are individual “studies” that prove what works for one particular patient, but they actually aren’t. And they are as likely to be wrong as right.
“I do not believe you have ever argued that anecdotal evidence is useless, so I am not inferring that is your stance.”
Correct. Anecdotes are a very weak kind of evidence with lots of bias and error built in, but they are useful when there is nothing better.
Thank you for this useful update! It will be especially interesting to see where the CBD research leads.
if someone has a internet link not behind a paywall that cbd oil in a randomized controlled trial using force plate measurement does not work please post a link. Chatgpt this morning is not aware of the study.
Searching for: cbd oil for dogs
Searching for: cbd oil for dogs
Generating answers for you…
Generating answers for you…
CBD oil is a natural oil extracted from the hemp oil plant, which is a variety of the Cannabis sativa plant species. It comes as broad-spectrum and full-spectrum CBD oil and used for oil in dogs or CBD edible treats for dogs. CBD is a non-psychoactive compound, meaning it does not produce the “high” associated with marijuana use1.
While there’s no definitive scientific data on using CBD to treat dogs, there’s anecdotal evidence from dog owners suggesting it can treat pain, especially neuropathic pain, as well as helping to control seizures2. The most typical uses for CBD oil for dogs include pain and anxiety management. When topically applied or ingested, it also has a soothing effect on some common skin conditions or mild irritations. CBD oil has also been used to help dogs who suffer from seizures as well as those who have been diagnosed with cancer3.
I hope this helps! Let me know if you have any other questions.
Received message. CBD oil is a natural oil extracted from the hemp oil plant, which is a variety of the Cannabis sativa plant species. It comes as broad-spectrum and full-spectrum CBD oil and used for oil in dogs or CBD edible treats for dogs. CBD is a non-psychoactive compound, meaning it does not produce the “high” associated with marijuana use. While there’s no definitive scientific data on using CBD to treat dogs, there’s anecdotal evidence from dog owners suggesting it can treat pain, especially neuropathic pain, as well as helping to control seizures. The most typical uses for CBD oil for dogs include pain and anxiety management. When topically applied or ingested, it also has a soothing effect on some common skin conditions or mild irritations. CBD oil has also been used to help dogs who suffer from seizures as well as those who have been diagnosed with cancer. I hope this helps! Let me know if you have any other questions.
Learn more:
1. honestpaws.com
2. akc.org
3. retrievist.akc.org
4. bestreviews.com
5. akc.org
+2 more
1
of
20
any randomized controlled trials treating dogs with cbd oil?
Sent message. any randomized controlled trials treating dogs with cbd oil?
Searching for: randomized controlled trials cbd oil dogs
Searching for: randomized controlled trials cbd oil dogs
Generating answers for you…
Generating answers for you…
Yes, there are some randomized controlled trials that have been conducted on the use of CBD oil for dogs. For example, a randomized, placebo-controlled clinical trial demonstrated that dogs with diagnosed osteoarthritis receiving a daily dose of only 0.3 mg per kg of proprietary CBD-infused oil formulation for four weeks showed significantly reduced pain and improved functional performance1. Another randomized blinded controlled clinical trial assessed the effect of CBD oil on seizure frequency in dogs and found that the CBD group received CBD-infused oil (2.5 mg/kg [1.1 mg/lb], PO) twice daily for 12 weeks in addition to existing antiepileptic treatments23.
I hope this helps! Let me know if you have any other questions.
Received message. Yes, there are some randomized controlled trials that have been conducted on the use of CBD oil for dogs. For example, a randomized, placebo-controlled clinical trial demonstrated that dogs with diagnosed osteoarthritis receiving a daily dose of only 0.3 mg per kg of proprietary CBD-infused oil formulation for four weeks showed significantly reduced pain and improved functional performance. Another randomized blinded controlled clinical trial assessed the effect of CBD oil on seizure frequency in dogs and found that the CBD group received CBD-infused oil (2.5 mg/kg [1.1 mg/lb], PO) twice daily for 12 weeks in addition to existing antiepileptic treatments . I hope this helps! Let me know if you have any other questions.
Learn more:
1. cannanine.com
2. pubmed.ncbi.nlm.nih.gov
3. avmajournals.avma.org
4. sciencedaily.com
5. pubmed.ncbi.nlm.nih.gov
+3 more
2
of
20
and that showed no effect
Sent message. and that showed no effect
Searching for: cbd oil dogs no effect randomized controlled trials
Searching for: cbd oil dogs no effect randomized controlled trials
Generating answers for you…
Generating answers for you…
I’m sorry but I couldn’t find any randomized controlled trials that showed no effect of CBD oil on dogs. However, there are some studies that have shown positive effects of CBD oil on dogs. For example, a randomized blinded controlled clinical trial assessed the effect of CBD oil on seizure frequency in dogs and found that the CBD group received CBD-infused oil (2.5 mg/kg [1.1 mg/lb], PO) twice daily for 12 weeks in addition to existing antiepileptic treatments1. Another study demonstrated that dogs with diagnosed osteoarthritis receiving a daily dose of only 0.3 mg per kg of proprietary CBD-infused oil formulation for four weeks showed significantly reduced pain and improved functional performance2.
I hope this helps! Let me know if you have any other questions.
skeptvet i think like chatgpt also is not aware of a force plate study using cbd oil so if chatgpt and skeptvet is not aware maybe there is none. My bad?http://skeptvet.com//2013/02/measuring-arthritis-pain-in-dogs-are-owner-surveys-as-good-as-force-plate-analysis/
Pingback: Arthritis Supplements for Dogs New Research Review – My Blog
So what are your thoughts on the supplement P. E.A it is now getting a lot of review and positive comments. There seems to be a lot of research that shows it actually works.
There is relatively little research on the use of this for arthritis in dogs, and no placebo-controlled blinded studies that I could find. Based on the preclinical research, it is plausible that it might help, but until clinical trials are done, that is just a hypothesis. I also only see one RCT in humans, and while that indicated a benefit, that too is pretty scant evidence, so I don’t think any firm conclusion is possible at this point.
Ok lets stop giving glucosamine for our dogs…but what should we do to manage arthritis in our dogs?
You wrote several articles on how glucosamine doesn’t work. Thank you for saving me money, but my dog still has arthritis and I still don’t know to help him.
Why not write more articles on studies that proved something that worked? So we know what to do?
Would love to know how to help/manage:
-allergies/itching
-anxiety
-aging
-how to prevent common diseases/health issues
As I explained in response to the same question on Twitter, the best source of science-based information about how to manage your personal pets’ arthritis is your veterinarian. The internet is not a substitute for individualized care.
There are some general guidelines for managing arthritis, and common elements are weight management, pain medication, and potentially physical therapy, which is clearly useful in humans but is only beginning to be studies in dogs and cats. The best option is to see your vet, have thorough and regular evaluations, including use of formal pain and mobility measurement tools such as the COAST, LOAD, or other such tools, and develop an individualized management plan for your pet.
Hello, I stumbled across your site. I’m perplexed that studies have found no benefit to glucosamine/chondroitin. I know this is just an anecdote but I had a 10 year old GSD who was struggling to stand or lay down with stiffness as she aged. After a week of glucosamine/chondroitin/MSM (suggested by my own vet) she was moving smoothly, and moved that way until her death at 12. The change was so striking that I have a hard time believing it could have been anything but the supplement. I am generally very against supplements not backed by science, but this one for me is hard to swallow that it doesn’t help senior dogs. Are we really saying it’s best to skip this supplement altogether in a senior dog with movement issues due to aging/arthritis?? I feel like, why not try it if it’s safely tolerated?
Despite being one of the most widely used (and profitable) supplements ever, decades of research have failed to show consistent, meaningful benefits. Things that actually have as dramatic an impact as it seemed to in your dog are not difficult to validate in research studies. Easy studies in antibiotics, for example, were a slam dunk because almost everyone taking them got better and almost everyone not taking them died! So if glucosamine supplements have any effect at all, it is pretty minor.
You are right they are very safe, so there is no compelling reason to give them up other than the wasted money. My biggest concern is that people often use these first before proven effective drugs for arthritis. I see dogs who have been in significant pain for years, but the caregiver placebo effect convinced their owners that they were better on the glucosamine, and this delayed truly effective treatment. That’s the real risk with supplements like this.
FWIW, there is actually a bit better evidence for fish oil in dogs with arthritis, so if you want to give a supplement, that’s more likely to help.
Skeptvet i just wanted to comment on your post above re “We really have no effective objective assessments” for musculoskeletal pain in cats. I think we are past that point. The Feline Musculoskeletal Pain Index (FMPI) has been validated and is useful both in a clinical and research setting. Accelerometers and activity trackers can be helpful in understanding differences in mobility, and the gold standard of pressure-sensitive walkways is available if those doing the research can afford the cost. Thanks 🙂
Thanks for the feedback!
Yes, there have been significant improvements in clinical metrology, and I do think CMIs such as FMPI are useful in research, though they have not been adopted by clinicians in real-world practice to any extent yet, apart from some use of pain scales.
So far, though, the use of activity trackers doesn’t seem to produce great data. The studies I have seen produce often unclear or contradictory results, especially inc ats. And objective tools like force-plate analysis are trick in dogs and notoriously difficult in cats, so I think we have a ways to go before we can consider those reliable even in research studies, and farther before we have pragmatic clinical practice tools for this.
I went through all of the “doctors” spiel and thought that it would be good for my pitbull. Within 2 weeks he started losing weight and had no energy. So, as these things worsened, we stopped giving him Dr Marty’s food and put him back on his regular food. He then started gaining weight back and was showing more energy. Within 2 weeks he was almost back to his old self. Dr. Marty’s food was killing my dog. It’s a fake. I would send the remainder of the food back and get my money back but I don’t have the order number that they require. Isn’t that a convenient way to get out of their guarantee?
Pingback: Senior Dog Arthritis Supplements: What you Need to Know - The Bridge Can Wait