Introduction
Cancer is a common disease in our pets just as it is in humans, though not necessarily for the reasons often claimed by proponents of alternative medicine. While there are certainly environmental triggers for many cancers, smoking being a classic and important example, it is not an established fact that we are facing an epidemic of cancer because we live in an “unnatural” and “toxic” environment.
For one thing, some toxic causes of cancer are actually less of a problem than in the semi-mythical “old days” before industrialization and modern science. Not too many chimney sweeps are getting scrotal cancer from soot these days, thanks to the identification and control of this risk through scientific research. And stomach cancer rates have fallen dramatically since the early 20thcentury, possibly due to less reliance on salting and smoking meats for preservation and the increased availability of fresh fruits and vegetables in urban areas, both consequences of technological advancement.
Perhaps more importantly, cancer is clearly a disease most often associated with old age, and one reason we see so much of it in humans and in our pets is that we, and they, and not dying as young as we used to of other things, like infectious disease and malnutrition.
Nevertheless, cancer is still a serious problem in our pets, and one which is being intensively studied in an effort to find effective prevention strategies and treatments. Again in contrast to the simplistic and inaccurate characterization of science-based cancer therapy, the reality is that there are effective therapies for many cancers, even cures for some, and these therapies consistently improve the length and quality of patients’ lives. Sure, we are a long way from preventing and curing cancer with the kind of success we’ve had preventing and curing infectious diseases, but the best hope for getting there is good, rigorous science.
Unfortunately, for individuals with pets who have cancer and who either don’t have good results with existing science-based therapies, or who are afraid of them due to the propaganda from proponents of alternatives, there are all too many untested snake oils freely available. There are far too many for me to evaluate them all, but occasionally I am asked to look at a specific product, and I feel it is important to remind desperate pet owners that even in the face of a terminal disease for which there is no proven cure, gambling on some concoction from the internet is risky. While it is not impossible that some of these products may work, it is less likely than the folks selling them would have you believe, for reasons which I will discuss.
And it is absolutely possible to make a bad situation worse with an untested treatment. Human patients with pancreatic cancer, which is highly aggressive and for which there are no truly effective conventional therapies, have unfortunately demonstrated this danger for us. Subjected to a bizarre diet, untested supplements, and coffee enemas under the Gonazalez cancer regime, these patients not only did not live as long as those on conventional therapy, they had significantly worse quality of life. Even in a situation where it seemed like they had ”nothing to lose,” a quack cancer therapy made these patients’ remaining days fewer and more uncomfortable than standard care. This is always a risk, for us and for our pets, with unproven treatments no matter how many testimonials and anecdotes companies give us to suggest their treatments are safe and effective.
An example of just such an untested therapy is Tumexal™.
What Is It?
As was the case for the equally “miraculous” and unproven kidney failure treatment RenavastTM I wrote about recently, the short answer is “Who knows?” Once again, the company selling this product refuses to disclose what it contains. This is a key warning sign for snake oil, and it is a clearly unethical way to promote a medical therapy. It is hard to imagine the public tolerating a pharmaceutical company trying to sell us a drug not only without any clinical studies to show it is safe and effective but without even disclosing what is in it, yet for some reason people tolerate this from companies selling mystery potions like TumexalTM. It is also, as the American Veterinary Medical Association (AVMA) Principles of Veterinary Medical Ethics states, unethical for veterinarians to foist such nostrums on their clients:
It is unethical for veterinarians to promote, sell, prescribe, dispense, or use secret remedies or any other product for which they do not know the ingredients.
Does It Work? Is It Safe?
The company has published a Powerpoint presentation claiming to explain the “science behind TumexalTM.” This presentation spends a lot of time describing one of many pathways to cancer formation, involving inactivation of the p53 tumor suppressor gene. The author then claims that TumexalTM stops cancer by inhibiting an enzyme called G6PD and that it “duplicates p53 function.” Without knowing what the substance is and with no published data showing if or how it does this, the truth of this claim cannot be evaluated. A recent published scientific paper discussing G6PD suppressors, however, does state ”To date, only a few G6PD inhibitors have been available. However, adverse side effects and high [concentration needed for a significant effect] hamper their use as therapeutics and basic research probes.” This argues against the claim that this company has found a perfectly safe and effective G6PD suppressor that the rest of the scientific community doesn’t know about.
Of course, the company behind TumexalTM has an explanation for why they have succeeded where the rest of the biomedical industry has not:
How is it that the scientists of CanineCare.US have come up with a treatment like Tumexal™, and not one of the big pharma drug houses?…Big pharma scientists are encumbered by a business model that insists in an absolute manner that every drug put into active development have billion dollar sales potential…Tumexal™ is a natural product for which a new composition of matter patent is not possible. But since CanineCare.US scientists are focused not on sales potential, but rather upon using cancer biology discoveries most effectively, we have been able to make progress far out of proportion to our numbers. Tumexal™ may never be a billion dollar drug, but it very well could help more dogs than all the billion dollar drugs of all the big pharma companies combined.
In other words, money-grubbing pharmaceutical companies have ignored the potential of safe and natural cancer treatments because they fear they won’t be able to patent and make any money off of them, but CanineCare.US is far more altruistic and doesn’t care about profits but only about making life better for your dog.
This is a common, and in this case completely incredible, explanation for the supposed story of a lone genius discovering a wonder drug. For one thing, there is plenty of profit potential in unpatentable “natural” products, which is why dietary supplements and herbal medicines are a multi-billion dollar industry that Big Pharma is actively interested in participating in. For another, the owner of this company, Jonathan Nyce, has already been a lavishly compensated CEO of a multi-million dollar pharmaceutical company, Epigenesis Pharmaceuticals, which forced him out when the supposedly revolutionary asthma drug he was developing failed to prove viable.** So the idea that pure altruism has motivated CanineCar.US to produce a wonder drug that the rest of the biomedical industry could not have found due to a blind pursuit of profit is not believable.
There are plenty of other warning signs of snake oil associated with this product. It is advertised primarily by sowing fear and distrust of conventional cancer therapy, exaggerating the dangers of chemotherapy, surgery, and radiation and completely ignoring the manifest benefits of conventional treatment. The slide show touting the product has all sorts of pictures of soldiers in WWI suffering the effects of chemical weapons and implies that because some chemotherapy drugs were developed based on these compounds that chemotherapy is merely “poisons as cancer medicine.”
The logic here is as flawed as it is simplistic. Smallpox and polio vaccines are made from smallpox and polio viruses, so are they simply “infections” the way cancer drugs are “poisons,” doing more harm than good? Many antibiotics are derived from bacteria and fungi, so are they automatically harmful “molds” with no real benefits? Of course not. Such therapies have dramatically reduced suffering and death for millions of people. The source of the medicine does not tell us anything about the balance of risks and benefits of the medicine itself. Only good scientific research can do this. Such research tells us what the pros and cons of cancer medicines are, but there is no such evidence to tell us the risks and benefits for TumexalTM.
Another red flag of quackery for TumexalTM are the claims of dramatic benefits with little to no risk.
TumexalTM : Effective, Safe Monotherapy for virtually all forms of Canine Cancer
Tumexal™ is also remarkable for its lack of harmful side effects. Unlike standard chemo drugs that can significantly reduce the quality of life in a treated dog, Tumexal™ is virtually toxicity free because of its novel mechanism of action.
And with Tumexal™ there is virtually no toxicity! In fact, Tumexal™ will almost always restore a cancer-stricken dog’s appetite, spirit and energy!
Such claims are always unlikely to be true, but when presented in the absence of any evidence and with a refusal even to disclose the ingredient in the drug, there is simply no reason to take them seriously at all.
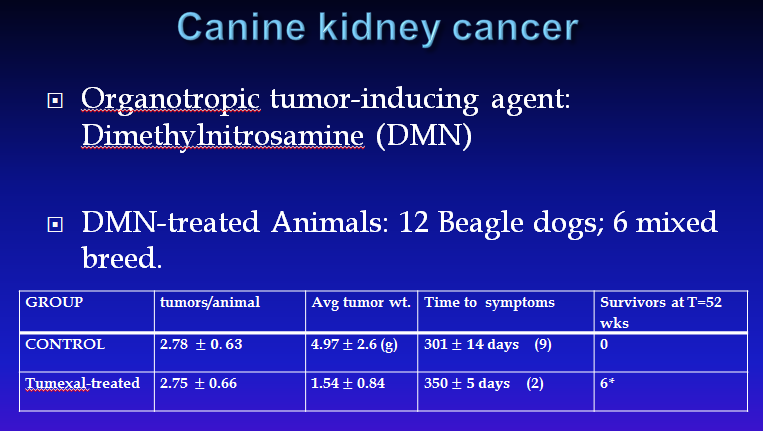
The Powerpoint Dr. Nyce has produced to sell the product does claim there is scientific research evidence that TumexalTM is effective, but this is highly suspect for several reasons. The evidence consists of a series of charts purporting to show laboratory beagles with cancer induced by researchers using toxic chemicals and then treated with TumexalTM or nothing. Invariably, they show that Tumexal works. Here is one example:
There is no evidence these experiments were ever published, or done at all for that matter. They also raise ethical questions about the use of these animals for fatal experiments since there is no information about the conduct of the studies or the care of the subjects, and since the studies were apparently never published to make the data useful to the scientific community but instead are used merely to promote a commercial product.
Dr. Nyce attempts to head off objections to these experiments by claiming “this work was done several decades ago using animals scheduled for destruction by animal control” and he “wouldn’t have the heart” to do this work today. Apart from the fact that this statement seems as implausible as the data themselves, it begs the question of why TumexalTM has only recently been developed, and only by Dr. Nyce, if extensive and costly research from decades ago produced such dramatic data that it is a potentially effective therapy for many cancers? Who did this research? Why was it not followed up? How was Dr. Nyce involved, if at all? Why was none of the data published?
All of this is highly suspicious, but of course impossible to evaluate objectively since the company does not provide any of the usual information, in the form of published research or regulatory documents, by which the value of potential new cancer therapies are judged.
What CanineCare.US does provide, of course, are testimonials, the sine qua non of quack therapies. Undoubtedly, people will comment on this post by saying I can’t prove TumexalTM doesn’t work, and lots of anecdotes show it does so what’s the problem? The problem, of course, is that such anecdotes and miracle stories prove nothing. They are available for every therapy ever invented, including many which have been definitively proven not to work, and they are deeply misleading. A responsible scientist and company generate and provide scientific data to show their products work, rather than simply posting heartwarming and meaningless anecdotes.
The defenses provided by CanineCare.US for their unproven claim, use of testimonials instead of data, and secrecy are self-serving and unconvincing. They amount to just a repetition of their claims, with no actual evidence provided, and snide denigration of the rest of the biomedical industry and anyone not willing to take the company at its word alone:
Very few people who have tried Tumexal have been disappointed in its results… It can extend life, and maintain a high quality of life, sometimes in dramatic fashion. It is important to note that every testimonial on our website is an authentic, unsolicited report from an owner whose dog has been treated with Tumexal. When cynics say that these testimonials are “too good to be true,” they are merely comparing them with the results they are accustomed to with traditional chemotherapy, or no treatment. In comparison, to such a cynic, the results obtained with Tumexal may indeed appear “too good to be true.”
A patent is not possible for Tumexal, because it is a natural product that nature, not us, synthesized… As a natural product for which a NCM patent is not possible, Tumexal must be protected by trade secret law. This is why we do not disclose what it is, except to say that it is natural.
So once again, we should believe TumexalTM is a wonder drug without any evidence other than the claims of the company selling it and the testimonials they choose to put on their web site because they are goodhearted people focused on making pets healthier rather than making money and the product is “natural.” Anyone who asks for more than this is a “cynic” who, by implication, doesn’t care about the welfare of pets or is beholden to Big Pharma. A finer modern example of snake oil could not be found. And it is worth remembering, the product from which the term “snake oil” likely derives didn’t work, and didn’t actually contain any snake oil! CanineCar.US and Dr. Nyce have given us no reason to think any better of TumexalTM.
Bottom Line
TumexalTM is yet another purported wonder drug with a “secret ingredient” that has been discovered by a lone genius and offered to the public out of altruism. It is supposed to be very effective and perfectly safe, and anyone who doesn’t take the company’s word for this is a “cynic” with questionable motives or a lack of compassion. Such claims are cheap and easy to make, but they are worthless without real scientific data, and none are available for TumexalTM. While it is impossible to prove it doesn’t work based on the nothing the company will tell us about it, it is not the job of skeptics to prove such wild, implausible claims untrue. It is the job of those who make them to prove they are valid. Anecdotes aren’t data, and cannot be used to prove a medical therapy is safe and effective. So to date, the company expects us to buy their product and administer it to our ill pets based only on their word for the safety and effectiveness of TumexalTM. Does this seem like a good idea?
And while the lack of definitive evidence against TumexalTM makes it impossible to assert it is ineffective, that doesn’t mean it can be assumed to be safe. Unproven remedies are as likely to hurt your pet as to help them, especially when substituted for real medicine. And even in the face of a disease as terrible as cancer, it is possible to make your pet’s life worse by rolling the dice on a snake oil like TumexalTM. If your pet has cancer, please see a veterinarian, ideally one specializing in cancer care. There really are beneficial treatments available even when there isn’t a cure.
If you are looking for information about pet cancer on the internet, watch out for snake oil peddlers. Here are some real experts with real information for you if your pet has cancer:
Veterinary Oncolink, University of Pennsylvania
Pet Owner’s Guide to Cancer, Cornell University
The Cancer Center at Cares, Canine Cancer Library, National Canine Cancer Foundation
Animal Cancer Center, Colorado State University
**There is a vivid tabloid story in Dr. Nyce’s life, complete with books by and about him, but since this has little bearing on whether or not the claims made about TumexalTM are legitimate, I did not include this material in my post.